- Rifampicin, also known as rifampin, is semi-synthetic derivative of rifamycin-B which is obtained from Streptomyces mediteranei. It is used to treat several types of bacterial infections.
- Rifabutin and rifapentine are structurally similar to rifampicin. These group of structurally similar macrolide antibiotics are known as rifamycin.
- Rifampicin was discovered in 1965, marketed in Italy in 1968 and approved to use in USA in 1971. It is available as generic medicine. It is included in World Health Organization’s List of Essential Medicines.
Mechanism of action of rifampicin
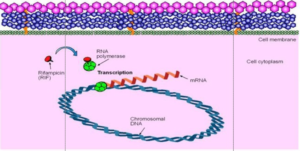
Figure 1- Mechanism of action of Rifampicin
- It is primarily bactericidal and has some bacteriostatic properties also. It binds to β subunit of bacterial DNA- dependent RNA polymerase forming stable drug-enzyme complex which suppress initiation of chain formation in RNA synthesis. This results in inhibition of RNA synthesis.
- It doesn’t inhibit human RNA polymerase. However, in large dose, it can inhibit RNA synthesis in mammalian mitochondria.
- Compared to isoniazid (INH), rifampicin is less bactericidal but has potent sterilizing activity.
Anti-bacterial spectrum of rifampicin
- It acts as bactericidal for both intracellular and extracellular microorganisms including tuberculosis and NTM (Non-tuberculosis Mycobacterium) such as M. kansasii and M. avium complex (MAC).
- It is also active against S aureus, S. albus, Cl. Welchii and M. leprae. Active as erythromycin or lincomycin against Streptococcus viridans, Pneumococci, Bacillus anthracis, C. diphtheriae, N. gonorrhoeae and meningococci. It is moderately active against S. faecalis and H. influenzae.
- It is active in-vitro against many gram-negative bacilli like coli, salmonella, Shigella and Brucella. However, they may develop resistance rapidly.
Resistance
- Resistance is caused by mutation in affinity of bacterial DNA dependent RNA polymerase for drugs which reduce drug binding to the polymerase.
- M fortuitum is highly resistant to rifampicin. Mycobacteria may rapidly develop rifampin resistance as a one-step process, and 1 of every 107–108 tubercle bacilli is resistant to the drug. Hence, rifampin should not be used alone.
Pharmacokinetics of rifampicin
- It is absorbed well after oral administration. Food interferes with its absorption. It is also available in parenteral form.
- Around 80% of drug binds to serum proteins, mainly albumin and is widely distributed in body tissues and fluids. The concentration attained in CSF (Cerebrospinal fluid) may be 10-20 % of blood concentration. It can cross placental barrier.
- Its half-life is between 1-5 hours.
- It is metabolized in liver to active metabolite desacetylrifampicin (more polar than parent compound) which undergoes enterohepatic circulation.
- Rifampicin and its metabolites are excreted mainly through the bile and into the feces. Small amount is excreted unchanged in urine. Dosage adjustment is not needed in patients with renal insufficiency.
- It imparts orange- red color to urine, feces and other secretions. Tears may stain soft contact lenses to orange- red. Patients should be informed about this before starting therapy.

Figure- Administration and fate of rifampicin (Source- Lippincott’s Illustrated Reviews, 6th edition)
Therapeutic Uses
- Used as first-line agent in treatment of tuberculosis. It is used as part of combination therapy with other anti-tuberculosis drugs like isoniazid, streptomycin and pyrazinamide.
- To treat leprosy.
- For prophylaxis of meningococcal disease and H. influenzae meningitis.
- Used in combination with β-lactam antibiotic or vancomycin to treat selected case of Staphylococcal endocarditis or osteomyelitis.
- To eradicate nasal staphylococci in patients with chronic furunculosis.
- In treatment of brucellosis.
- To treat legionnaire’s disease.
Adverse Effects
- In usual doses, around 4-5 % of patients may experience adverse effects like rashes, fever, nausea and vomiting. It also causes jaundice, proteinuria, leucopenia and thrombocytopenia.
- Hepatitis may occur. Chronic alcoholism, old age and chronic liver disease increases risk of severe hepatitis when rifampicin is used alone or in combination with isoniazid. It is recommended to check hepatic function before starting the therapy.
- Large doses of rifampicin (˃900 mg) used intermittently can cause acute hepatic and renal failure, allergic reaction including shock and flu-like syndrome.
- CNS symptoms include headache, fatigue, drowsiness, dizziness, inability to concentrate, pain in extremities, confusion and generalized numbness.
Drug Interaction
- As it is potent inducer of hepatic CYPs, it can increase metabolism of several drugs including:
- Phenytoin
- Oral anticoagulants including warfarin
- Sulfonylurea
- Oral contraceptives
- Theophylline
- Simvastatin
- Protease inhibitors including ritonavir, indinavir and lopinavir and non-nucleoside reverse transcriptase inhibitors (NNRTIs) including nevirapine and efavirenz.
- Propranolol and metoprolol
- Glucocorticoids
- Digoxin
- Dapsone
- Barbiturates
- Halothane
- Anti-arrhythmic drugs like quinidine and tocainide.
- While co-administering with above mentioned drugs, it may be necessary to increase dose of these drugs or switch to drugs less affected by rifampicin.
Contraindication
- It is better avoided during pregnancy and breastfeeding.
- Contraindicated in patient allergic or hypersensitive to rifampicin.
- It is contraindicated in patients with hepatic impairment, jaundice, biliary obstruction or porphyria.
- Used with caution in alcoholics and malnourished patients.
Reference
- Goldstein BP. Resistance to rifampicin: a review. The Journal of Antibiotics. 2014; 67: 625–630.
- Acocella G. Clinical pharmacokinetics of rifampicin. Clin Pharmacokinet. 1978; 3(2): 108-27.
- Stott KE, Pertinez H, Sturjenboom MGG, BOeree MJ, Aarnoutse R, Ramachandran G et al. Pharmacokinetics of rifampicin in adult TB patients and healthy volunteers: a systematic review and meta-analysis. J Antimicrob Chemother. 2018; 73(9): 2305–2313.
- https://en.wikipedia.org/wiki/Rifampicin
- https://www.medicineindia.org/pharmacology-for-generic/436/rifampicin
- Pharmacology and Pharmacotherapeutics. 24th edition.
- A Textbook of Clinical Pharmacology and Therapeutics.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.