- Streptomycin is first aminoglycoside antibiotic to be discovered and is used in medical field since 1940s. It is originally obtained from soil organism Streptomyces griseus.
- Streptomycin is available as sulphate salt of streptomycin. Its use is declined nowadays due to development of resistance and toxicity.
Indications of streptomycin
- Tuberculosis– Previously, it was used as first and most effective agent in treating pulmonary tuberculosis in combination with other agents like isoniazid, pyrazinamide and ethambutol. However nowadays, it is used as alternative to current standard therapy of RIPE (Rifampicin, Isoniazid, pyrazinamide and ethambutol). It is used if RIPE therapy is unavailable or cannot be tolerated by patient.
- Plague– It is the drug of choice in treatment of plague. It is used even in children and old people with pneumonic plague.
- Used to treat tularemia and brucellosis.
- Bacterial endocarditis– Used to treat serious enterococcal infections, group D streptococci and oral streptococci of viridans group in combination with penicillin G. It is replaced by gentamicin but is preferred when targeted strain is not sensitive to gentamicin.
Antibacterial spectrum of streptomycin
- It exerts bacteriostatic effect in low concentration and bactericidal effect in high concentration. Its bactericidal action is concentration dependent; there is progressive increase in bactericidal action along with concentration.
- Streptomycin is effective against aerobic gram-negative bacteria and some gram- positive bacteria. It is effective against M. tuberculosis, E. Coli, Pseudomonas aeruginosa, Aerobacter aerogenes, Brucella, Lisetria and Nocardia. Its effectiveness against P. aeruginosa is less compared to other aminoglycoside antibiotics like gentamicin and tobramycin. Organisms like salmonella, Staphylococci, Strep. Pyogens, S. viridae are moderately sensitive to streptomycin.
Resistance
- Its wide spectrum of activity has diminished to development of antibiotic resistance. Mechanisms involved are
- decreased cell permeability to antibiotic which prevent drug from reaching the ribosomes.
- Single step mutation which affect ribosomal proteins. This is uncommon and is specific for streptomycin.
- R factor mediated resistance which means drug inactivation by modifying enzymes acquired by conjugative transfer of R plasmids.
Mechanism of action of streptomycin
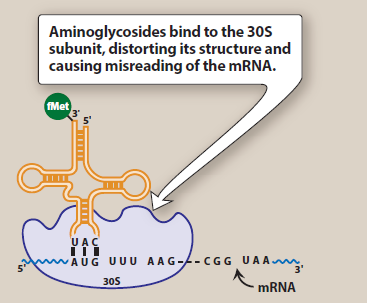
Figure- Mechanism of action of streptomycin (aminoglycoside antibiotics) (Source- Lippincott’s Illustrated Reviews)
- Like other aminoglycosides, it also acts by inhibiting protein synthesis. It diffuses through porin channels of gram-negative bacteria and enter periplasmic space. Once inside the cell, it binds to side of 16S rRNA of 30S ribosomal subunit and interfere with protein synthesis initiation, block translation of m-RNA and prematurely terminate the synthesis.
- They cause misreading of genetic code by 30S ribosomal subunit leading to production of abnormal proteins. These proteins when inserted into the cell membrane results in alteration of permeability, disruption of cell membrane and further stimulate aminoglycoside transport.
Pharmacokinetics
- It is administered via IV or deep IM injection. When given through IM route, peak plasma level is achieved within 30- 60 minutes and the activity lasts for 6-8 hours. Oral route is not preferred due to poor absorption.
- Its serum half-life is around 2.5 hours. It is distributed mainly into lean tissues. Hence, in obese patients its dose is calculated based on ideal body weight, not based on total body weight. It is diffused into synovial, peritoneal and pericardial fluid. To achieve high concentration in pleural fluid, repeated systemic administration is required. It crosses placental barrier. It doesn’t cross BBB, but sufficient concentration is achieved in CSF (cerebrospinal fluid) in case of meningeal inflammation.
- Excretion takes place mainly via urine. Around 50-60 % is excreted unchanged via urine within 24 hours. Its half-life may increase by 50 to 100 hours in patients with renal impairment.
Adverse effects
- It has narrow therapuetic index similar to other aminoglycosides. Hypersensitivity reactions are common and can manifest as rashes, eosinophilia and fever. Serious manifestations like blood dyscrasias, angioedema occur rarely. It can cause pain at site of injection.
- The most serious adverse effect is eighth cranial nerve damage. It can cause reversible impairment of vestibular function. It can cause permanent hearing loss. Chances of developing ototoxicity is more in infants, elder people and in patients with impaired renal function.
- Nephrotoxicity is another common adverse effect which occurs due to accumulation and retention of streptomycin in proximal tubular cells. It can cause mild albuminuria or acute tubular necrosis. Chances of azotemia is rare.
- Acute neuromuscular blockade may occur due to rapid increase in concentration or concurrent administration with neuromuscular blockers. Patients with myasthenia gravis are more susceptible. It may be reversed with calcium gluconate infusion or by neostigmine.
- It can also cause optic neuritis and peripheral neuritis. Chances of superinfection with Candida and Staph. aureus is also reported.
Drug Interaction
- When used in combination with chloramphenicol, chances of developing optic neuritis increases. So, it is not generally combined with chloramphenicol.
- Concurrent administration with neuromuscular blockers may cause acute neuromuscular blockade.
Contraindication
- Used with caution in patients with renal impairment and in elderly patients.
- Contraindicated in following condition:
- Patients with myasthenia gravis.
- In patients who are allergic to streptomycin.
- In pregnancy as it can cross placenta with its ototoxic effects.
References
- Streptomycin – StatPearls – NCBI Bookshelf (nih.gov)
- https://go.drugbank.com/drugs/DB01082
- https://www.rxlist.com/streptomycin-drug.htm#clinpharm
- https://www.britannica.com/science/streptomycin
- Reference Module in Life Sciences. Brenner’s Encyclopedia of Genetics (Second Edition). 2013: 568-569.
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- A Textbook of Clinical Pharmacology and Therapeutics.
- Goodman and Gillman’s Manual of Pharmacology.