Introduction
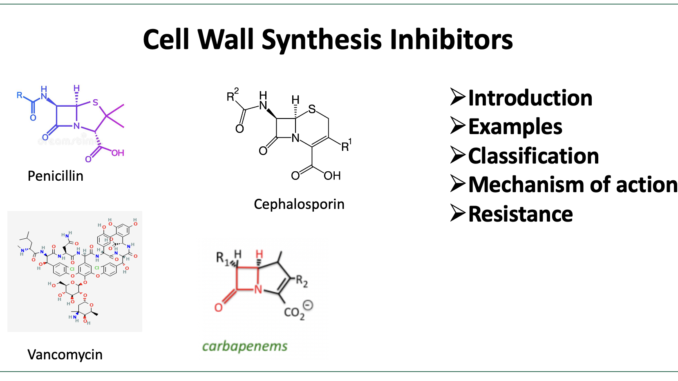
- Cell wall synthesis inhibitors are one of the most important and effective classes of antibiotics. The most important members of cell wall synthesis inhibitors are beta-lactam antibiotics and glycopeptides. Beta-lactam antibiotics are named after the beta-lactam ring which is required for their activity. Penicillin which is the first antibiotic discovered is a member of beta-lactam antibiotics. Vancomycin is the first glycopeptide antibiotic approved for medical use.
- Some examples of cell wall synthesis inhibitors include penicillin, cephalosporin, vancomycin, etc.
Classification
- Beta-lactam antibiotics and glycopeptides are two major classes of antibiotics that produce their effect by inhibiting bacterial cell wall synthesis.
Beta-lactam antibiotics
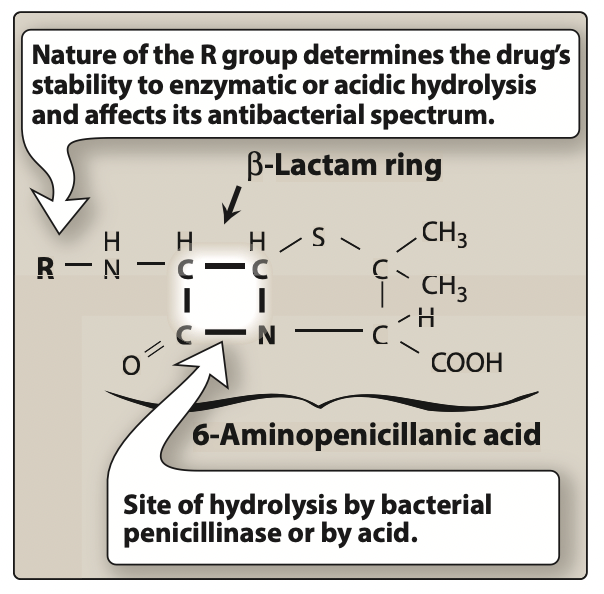
Figure- Structure of beta-lactam antibiotics (Source- Lippincott’s Illustrated Reviews, 6th edition)
- Penicillin- Penicillin G, Penicillin V, Amoxicillin, Nafcillin, Oxacillin, Ticarcillin.
- Cephalosporins– Cefazolin, Cefdinir, Cefixime, Cefotazime, Cefotetan, Cefprozil.
- Carbapenems– Doripenem, Ertapenem, Imipenem, Meropenem.
- Monobactams– Aztreonam.
Glycopeptides
Vancomycin, Daptomycin, Linezolid, Mupirocin, Retapamulin.
Bacterial cell wall and its synthesis
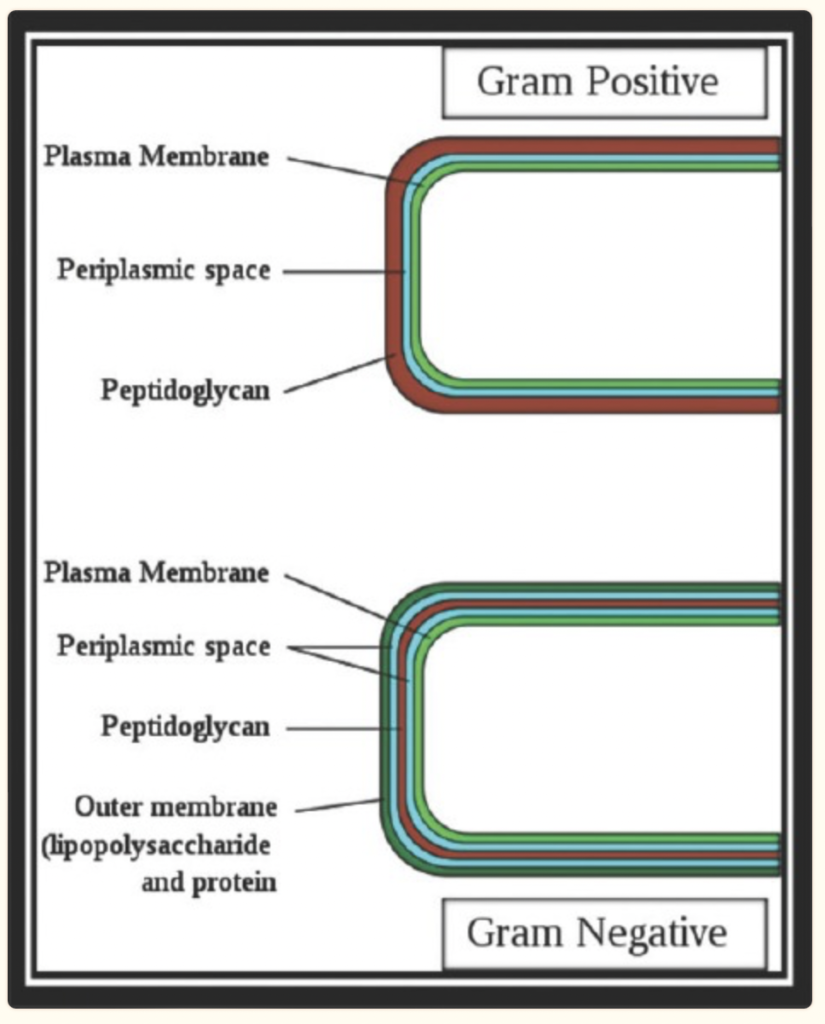
Figure- Structure of bacterial cell envelope
(Source- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5672523/)
- The cell wall is one of the important features that differentiate mammalian and bacterial cells. It plays a major role in stress-bearing and shape maintenance in bacteria. The cell wall is present in both gram-positive and gram-negative bacteria and consists of cross-linked polymer peptidoglycan.
- Peptidoglycan, which is also called murein, is a polymer and consists of polysaccharide strand which is cross-linked via short peptide bridges. Its synthesis is a complex process that occurs in three major steps in the cytoplasm, on the inner side and outer side.
- Cytoplasmic steps consist of the synthesis of nucleotide precursors which includes the formation of UDP-GlcNAc (N- acetylglucosamine), UDP-MurNAc (N-acetyl muramic acid), assembly of peptide stem, and synthesis of D-glutamic acid and D-alanyl-D-alanine. The second step involves the formation of lipid intermediates like lipid I and lipid II. In the third stage, which occurs in periplasmic space, the precursors formed in the first and second steps are polymerized into the peptidoglycan layer. Penicillin Binding Proteins (PBPs) are involved in 3rd step. They are involved in the polymerization of glycan strands and cross-linking between glycan chains.
Process of Inhibition
- Beta-lactam antibiotics bind to penicillin-binding proteins and inhibit cell wall synthesis. PBP mistake the beta-lactam ring of these antibiotics as their substrate- D-Ala-D-ala of the pentapeptide terminal. Serine residue of the active site of PBP binds to the carbonyl of the b-lactam ring, cleaves the ring, and forms an inactive acyl-enzyme. This inactive acyl-enzyme has a long lifetime. Hence, b-lactam inhibits any further nucleophilic attack on the active site of PBPs which leads to the inhibition of crosslinking of the peptidoglycan layer by PBPs.
- Glycopeptide antibiotics are glycosylated tricyclic or tetracyclic heptapeptides which target lipid II. First-generation glycopeptide antibiotics like vancomycin and teicoplanin bind to acyl-D-alanyl-D-alanine in lipid II and prevent further polymerization of the peptidoglycan layer. Some drugs of this class like corbomycin and complestatin bind to peptidoglycan, inhibit autolysins, and prevent cell division.
Mechanism of Resistance
- Resistance towards beta-lactam antibiotics may develop through:
- Production of b-lactamase enzymes which causes enzymatic cleavage of b-lactam ring. So, b-lactamase inhibitors like clavulanic acid, tazobactam, sulbactam are used b-lactamase sensitive antibiotics. They don’t have significant antibacterial activity on their own. However, they can bind to and inactivate b-lactamase and protect b-lactamase-sensitive antibiotics.
- Modification of target PBPs. Changes in the active site of PBPs result in the lower affinity of b-lactam antibiotics for PBPs.
- Decreased penetration of these drugs to target PBPs.
- Efflux pumps can reduce the amount of intracellular drugs and confer resistance.
- Previously, it was thought that it was difficult to develop resistance against glycopeptide antibiotics. Resistance against vancomycin was observed in Enterococci after 30 years of approval of vancomycin. The incidence of vancomycin-resistant enterococci (VRE) is increasing in hospitalized patients. The resistance was developed due to the transfer of resistance genes from other glycopeptide-resistant bacteria. The first case of vancomycin-resistant S. aureus was reported in 2001. To prevent the increase in the number of other vancomycin-resistant bacteria, the use of vancomycin should be restricted for serious infections.
References
- Dorr T, Moynihan PJ, Mayer C. Bacterial cell wall structure and dynamics. Front. Microbiol. 2019; 10 (2051): 1- 4.
- Zhou J, Cai Y, Liu Y, An H, Deng K, Ashraf Ma, et al. Breaking down the cell wall: still an attractive antibacterial strategy. Front. Microbiol. 2022; 13 (952633): 1-21.
- Kapoor G, Saigal S, Elongavan A. Action and resistance mechanisms of antibiotics: A guide for clinicians. J Anaesthesiol Clin Pharmacol. 2017; 33: 300-5.
- Scheffers DJ, Pinho MG. Bacterial cell wall synthesis: new insights from localization studies. Microbiol Mol Biol Rev. 2005 Dec;69(4):585-607.
- Lippincott’s Illustrated Reviews Pharmacology. 6th edition.