- Cardiac arrhythmia is defined as disturbance of initiation or conduction of cardiac impulse.
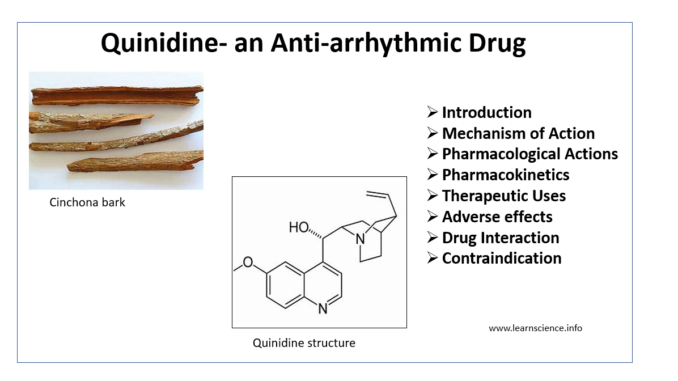
- Quinidine is an isomer of antimalarial drug quinine, originally isolated from bark of cinchona tree and has very long history as anti-arrhythmic agents. It had been used in treatment of almost all cardiac arrhythmias (especially atrial fibrillation) since 20th century.
- It is said that a French physician Jean- Baptiste de Senac was first to document anti-arrhythmic effect of cinchona bark in mid-18th century. Later, Wenckebach- an Austrian cardiologist encountered a patient who abort his atrial fibrillation attacks by using quinine and hence introduced quinine as anti-arrhythmic drug.
- Quinidine belongs to Group IA anti-arrhythmic agent. Other drugs belonging to this group are procainamide and disopyramide.
Mechanism of action of Quinidine
- It binds to open and inactivated sodium channels and prevent sodium influx required for initiation and conduction of impulse. Thus, it delays initial rapid depolarization and slow the phase 0 depolarization rate resulting in slow conduction velocity.
- It prolongs repolarization (refractoriness, phase 3) and hence prolong the action potential duration.
- Quinidine also possess mild α-adrenergic blocking and anti-cholinergic actions.

Figure 1- Schematic diagram of effects of class IA antiarrhythmic agents including quinidine. (source- Lippincott’s Illustrated Reviews. 6th edition)
Pharmacological actions of Quinidine
Cardiac Actions
- Quinidine depress excitability of cardiac tissues, depress diastolic depolarization and hence, automaticity.
- It slows conduction velocity and prolongs repolarization, has negative ionotropic action on heart.
- It causes unpredictable abnormalities of rhythm in digitalized heart.
Extra Cardiac actions
- Quinidine lowers BP in most patients.
- It depresses skeletal muscle. It shows antimalarial, antipyretic and weal oxytocic activities like quinine.
Pharmacokinetics
- Quinidine sulphate or gluconate is rapidly and completely absorbed after oral administration.
- After a single oral dose, peak effects are reached within 2-3 hours and lasts for 6-8 hours. It binds extensively to plasma protein like albumin.
- It undergoes extensive metabolism in liver. So, it interacts with drugs that induce or inhibit liver enzymes. One active metabolite 3-hydroxyquinidine is as potent as quinidine itself.
- About 20-25 % of drug is excreted unchanged in urine.
- Quinidine clearance is affected very less in patients with renal damage and congestive heart failure. So, dosage requirement is like other patients.
Therapeutic Uses of Quinidine
- Used in treating wide variety of arrhythmia including atrial, AV junctional and ventricular tachyarrhythmia.
- In atrial fibrillation and atrial flutter.
- In atrial, nodal and ventricular premature beats.
- Quinidine sulphate is used to treat malaria.
Adverse Effects
- It is poorly tolerated. It could be very toxic if given through IV route.
- Diarrhea is most common adverse effect occurring in 30-50% of patients. Diarrhea induced hypokalemia can increase risk of torsades de pointes (specific type of abnormal heart rhythm which can lead to sudden cardiac death).
- 2-5 % of patients receiving quinidine therapy develops torsades de pointes and QT interval prolongation.
- It produces cinchonism as a result of cumulative over dosage. The symptoms include ringing in ears, light-headedness, giddiness, vertigo and blurred vision. It can be managed by dose reduction.
- Cardiac toxicity includes bradycardia, conduction defects and heart failure. Patients with marked cardiac damage are at more risk. Hypotension is more common in older patients.
- Allergic reactions like skin rashes, fever and thrombocytopenic purpura may occur.
Drug Interaction
- It interacts with drugs that either inhibit or induce liver enzymes.
- Drugs which increase amount of quinidine by inhibiting liver enzymes include:
– Antacids like sodium bicarbonate and cimetidine.
-Antifungal drugs like ketoconazole.
- Drugs that decrease amount of quinidine in blood by inducing liver enzymes includes:
- Antiseizure medicines like phenytoin and phenobarbital.
- Anti-hypertensive medicines like propranolol, nifedipine and verapamil.
- Antibiotics like rifampin.
- Quinidine increase concentration of drugs like warfarin, antipsychotic drugs like haloperidol and antidepressant drugs like amitriptyline and imipramine.
- It decreases blood concentration of drugs like codeine and hydrocodone.
Contraindications
It is contraindicated in:
- History of quinidine intolerance.
- Hypotension.
- Myasthenia Gravis.
- Stokes- Adams syndrome.
- QT prolongation.
- Chronic Heart Failure.
Note- Nowadays quinidine is not widely prescribed for many reasons: treatment carries a risk of potentially fatally adverse effects, most patients will develop gastrointestinal side effects which can become intolerable; and the drug is no longer under patent and so not commercially promoted.
References
- Roden DM. Pharmacology and Toxicology of Nav1.5-Class 1 anti-arrhythmic drugs. Card Electrophysiol Clin. 2014; 6(4): 695–704.
- Grace AA, Camm AJ. Quinidine. N Engl J Med. 1998; 338: 35-45.
- Serdoza LV, Rittgera H, Furlanellob F, Bastiana B. Quinidine—A legacy within the modern era of antiarrhythmic therapy. Pharmacological Research. 2019; 144: 257-263.
- Hemel N. Quinidine rehabilitated and more lessons from the PAFAC and SOPAT anti-arrhythmic drug trials for the prevention of paroxysmal atrial fibrillation. European Heart Journal. 2004; 25(16): 1371–1373.
- Cardiac Intensive Care. 3rd Pages 432-445. e7.
- Cardiac Electrophysiology: From Cell to Bedside. 7th Pages 1062-1075.
- Lippincott Illustrated Reviews Pharmacology, 6th
- Goodman and Gillman’s Manual of Pharmacology.
- Pharmacology and pharmacotherapeutics. 24th