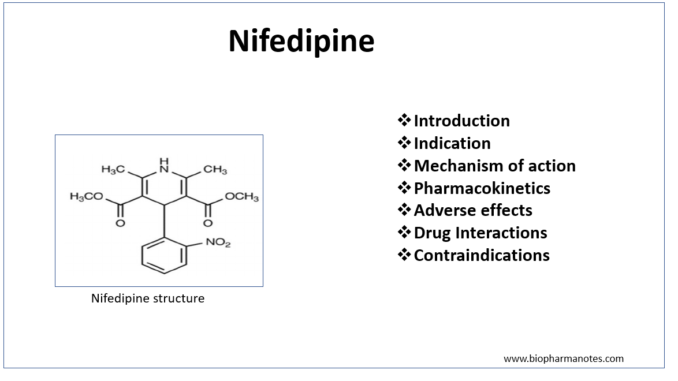
- Nifedipine is calcium channel blocker (CCBs) belonging to dihydropyridine class. Calcium channel blocker (CCBs) also known as calcium channel antagonist or calcium antagonist are group of medicines that block movement of calcium through calcium channel.
- It was approved by FDA for medical use in 31 December 1981. It is also available as generic medicine and is included in World Health Organization’s List of Essential Medicines.
Indications of nifedipine
- Used in hypertension as monotherapy or in combination with other anti-hypertensive agents.
- In chronic stable angina and vasospastic angina.
- Some off-label uses are
- Raynaud’s phenomenon
- Pulmonary arterial hypertension
- Achalasia
- Tocolysis
- High altitude pulmonary edema.
Mechanism of action of nifedipine
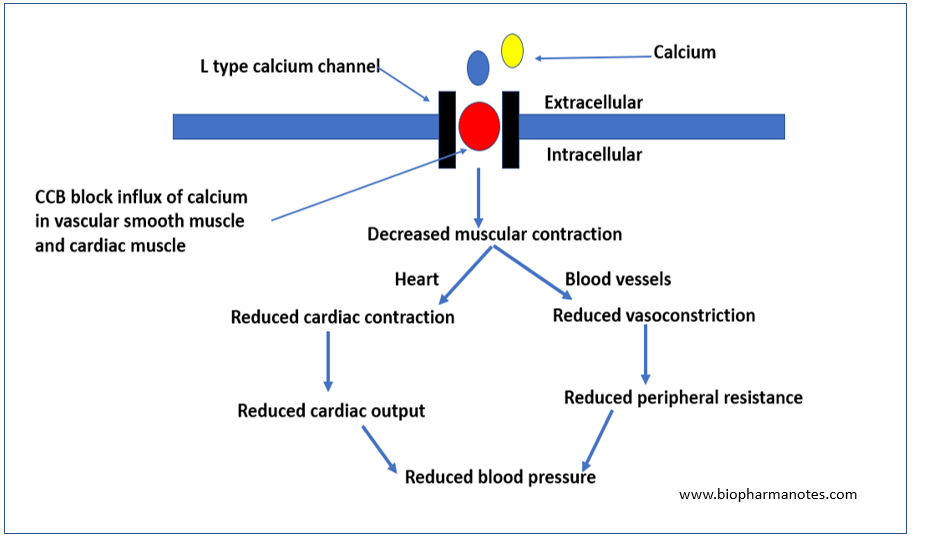
- Its mechanism of action is similar to other CCBs i.e. by blocking L- type calcium channel.
- Calcium play important role in excitation-contraction coupling in the skeletal, cardiac and smooth muscle. The contractility of cardiac and vascular smooth muscle is highly dependent on extracellular calcium.
- There are two types of calcium channel in heart: L channel and T channel.
- Nifedipine binds to alpha-1 subunit of L channel and inhibit entry of calcium into cardiac and vascular smooth muscle. This causes decrease in intracellular calcium leading to relaxation of vascular smooth muscle, vasodilation and ultimately reduce blood pressure. It reduces contraction in cardiac muscle and slows sinus pacemaker and AV conduction.
Pharmacological actions of nifedipine
- It causes selective relaxation of arterial resistance vessels. This results in lowering of arteriolar resistance and blood pressure, improves contractility and segmented ventricular function. It also slightly increases heart rate and cardiac output.
- It causes relaxation of bronchial, uterine and ureteric smooth muscle.
- When compared to verapamil, it:
- Has more potent coronary and peripheral vasodilation effect.
- Is potent inhibitor of platelet aggregation.
- Possess negligible negative ionotropic effect.
- Causes tachycardia.
Pharmacokinetics
- Administered by oral or sublingual route. It is available both as immediate and sustained release preparation. Extended release preparation is available as 30, 60 and 90 mg tablets. The onset of action for immediate release preparation is around 20 minutes.
- Its bioavailability is 40-70% and have plasma half-life of 2-5 hours. Plasma half-life in case of extended release may be around 24 hours.
- It is metabolized in liver by CYP3A4 pathway to inactive or weakly active metabolites. Dosage adjustment is needed in hepatic patients.
- It is excreted mostly in urine as inactive water-soluble metabolites (around 60-80%). Remaining percentage is excreted via feces.
Adverse Effects
- Adverse effects occur due to vasodilatory properties of nifedipine and occur in about 20-30 % of patients. Many of adverse effects of nifedipine are related to its peak plasma half-life. Extended release preparation of nifedipine has improved its safety profile.
- Some common adverse effects include headache, dizziness, flushing and peripheral edema.
Drug Interactions
- Nifedipine when administered together with products containing grapefruit juice, can affect heart rate and blood pressure. Grapefruit downregulate expression of CYP3A4 enzyme which play important role in metabolism of nifedipine. This increases level of nifedipine and can cause headache and dizziness. So, grapefruit juice should be avoided while taking nifedipine.
- Nifedipine reduces hypoglycemic potency of acarbose. Concurrent administration with drugs like aliskiren may increase risk of hyperkalemia.
- Its metabolism can be increased by concurrent administration with vinca alkaloids like vincristine, vinblastine and vindesine.
Contraindications
- Contraindicated in patients hypersensitive to nifedipine.
- Immediate release preparations of nifedipine is avoided in patients with hypertensive emergencies.
- It is contraindicated in patients with severe aortic stenosis, hypotension and heart failure.
- It is avoided in patients with hepatic impairment.
References
- https://www.ncbi.nlm.nih.gov/books/NBK537052/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2663456/
- Elliott WJ, Ram VS. Calcium Channel Blockers. The Journal of Clinical Hypertension. 2011; 13(9): 687-689.
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- A Textbook of Clinical Pharmacology and Therapeutics. 5th edition.