• Beta-blocker (β-blocker) also known as beta-adrenergic blocking agent, are one of the most extensively used medicine for cardiac and non-cardiac disorders.
• The first clinically significant β-blocker, propranolol and pronethalol were synthesized in 1964. Propranolol was approved by FDA for treatment of angina in 1973. This revolutionized the management of angina pectoris and is considered one of the most important achievement of medical field in 20th century.
•Name of most beta-blockers ends in -olol except some like carvedilol.
Classification of beta-blockers
1) Cardio selective β-1 blocker: Examples are atenolol, metoprolol, esmolol, acebutolol and bisoprolol.
2) Non-selective β-1 and β-2 blocker: Examples are propranolol, timolol, sotalol and carteolol.
3) Beta-blocker with additional properties: Examples are labetolol, carvedilol, betoxolol and nebivolol.
Mechanism of action of beta-blockers

Figure 1- Mechanism of action of beta-blockers
• They block beta-receptors and prevent binding of epinephrine and nor-epinephrine to beta-receptors. Epinephrine and nor-epinephrine are neurotransmitters.
• There are 3 kinds of beta-receptors:
Beta-1 (β-1) receptors are present in heart, eye and kidneys.
Beta-2 (β-2) receptors are present in lungs, GI tract, uterus, blood vessels and skeletal muscles.
Beta-3 (β-3) receptors are present in fat cells.
• They mainly affect β-1 and β-2 receptor and hence block actions of epinephrine and nor-epinephrine.
Pharmacological Actions of beta-blockers
Cardiac effects
• They don’t have affect on normal heart when subject is at rest.
• In case of increased sympathetic tone, they slow A-V conduction, reduce myocardial contraction, cardiac output, automaticity and prevent rise in heart rate.
• They reduce myocardial oxygen requirement and hence, improve exercise tolerance.
• Some β-blockers like propranolol, when used in higher concentration, has direct depressant effect on heart.
Blood pressure
• Non-selective blockade of βeta receptors block β-2 mediat vasodilation in skeletal muscle. They reduce cardiac output. These helps in reduction of both systolic and diastolic blood pressure in hypertensive patient.
• They don’t cause postural or exercise induce hypotension (as alpha-2 adrenergic receptors are not blocked).
• During chronic use, they decrease total peripheral resistance.
Bronchoconstriction
• Blockade of β-2 receptor in bronchi and bronchioles cause contraction of bronchial smooth muscles. This may be harmful in patients with asthma and COPD (Chronic Obstructive Pulmonary Disease).
• So non-selective β-blockers are contraindicated in asthma or COPD.
Metabolic effect
• They can modify carbohydrate and lipid metabolism.
• Chronic use may cause increase in LDL cholesterol and triglycerides and decrease in HDL cholesterol. Selective β -1 blocker may improve lipid profile.
Intra-ocular pressure (Eye)
• When applied orally or topically, they reduce intraocular pressure by reducing secretion of aqueous humour.
CNS
• Lipid soluble β-blocker like propranolol, labeatolol and metoprolol can cross BBB (Blood Brain Barrier). Propranolol alters mood and is used in anxiety.
Pharmacokinetics of beta-blockers
• All β -blocker differ in their pharmacokinetic properties.
• The effective oral dose range of β-blockers are wide. Some β-blockers like propranolol and metoprolol undergoes first pass metabolism, so their oral bioavailability is low. The relative oral bioavailability of sotalol and pidolol is better.
• Plasma half of those β-blocker which are metabolized by liver is short (2-3 hours) and of those excreted unchanged is long (8-12 hours).
• Duration of action is modified by active metabolite, presence of liver and kidney disease.
• The plasma t½, does not correlate well with the duration of their therapeutic effects. This is because the plasma level declines exponentially and follow first order kinetics while the therapeutic effect decreases linearly, following zero order kinetics. Hence, most agents can be given orally at much longer intervals than is suggested by their plasma half-lives.
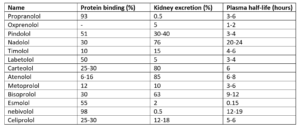
Table 1- Pharmacokinetic parameter of some beta-blockers (source- Pharmacology and Pharmacotherapeutics, 24th edition)
Therapeutic Uses
• Mainstay of chronic, prophylactic treatment of angina pectoris.
• In myocardial infarction.
• As class II anti-arrhythmic agent.
• In hypertension. (nowadays not used as first-line therapy for hypertension) and heart failure.
• In pheochromocytoma (tumor of adrenal gland). For patients with pheochromocytoma, α adrenergic blockers are used before surgery. In some patients, however, α blockade leads to a severe tachycardia particularly when atropine is used for preanesthetic medication. Propranolol, in the dose of 1-5 mg IV prevents this complication.
• In hypertrophic obstructive cardiomyopathy and chronic open-angle glaucoma.
• Used as adjunct with anti-thyroid drugs in thyrotoxicosis.
• To control withdrawal symptom in alcohol addict.
• Prevention of migraine.
Adverse Effects
• Common side effects include fatigue, lethargy, headache, confusion, blurred vision, insomnia, hallucination, nausea and vomiting. Hypotension and excessive bradycardia may occur.
• Some serious side effects are bronchospasm (mainly in patients with asthma), Raynaud’s phenomenon, toxic epidermal necrolysis, Steven Johnson syndrome, lupus erythematous and serious allergic reactions.
• They may also cause sexual dysfunction.
• They mask the symptoms of hypoglycemia in people with diabetes. So, in patients with diabetes mellitus, cardio selective β-blockers are used.
• When withdrawn suddenly, they may worsen angina, cause serious heart attack or sudden death. So, the dosage should be reduced gradually.
Drug interaction
• Combining propranolol or pindolol with chlorpromazine interfere with each other’s elimination and result in hypotension.
• Phenobarbital may increase breakdown of propranolol and metoprolol and reduce their effectiveness.
• Combination of clonidine and beta-blocker may elevate blood pressure dangerously. Discontinuation after their concurrent use also have same effect.
• NSAIDs like aspirin and ibuprofen counteract with blood pressure reducing effect of beta-blockers.
Contra-indication
They are contraindicated in:
• Asthma and COPD.
• Severe bradycardia.
• In severe bronchospasm and severe depression.
• Cardiogenic shock.
• Raynaud’s phenomenon.
• Diabetic patient on insulin.
• In left ventricular failure.
References
1) Talbert RL. Pharmacokinetics and Pharmacodynamics of Beta Blockers in Heart Failure. Heart Failure Reviews. 2004;9: 131-137.
2) Ripley TL, Saseen JJ. β-blockers: A Review of Their Pharmacological and Physiological Diversity in Hypertension. Ann Pharmacother. 2014; 48(6): 723-33.
3) DiNicolantonio JJ, Fares H, Niazi AK, Chatterjee S, D’Ascenzo F, Cerrato E, Biondi-Zoccai G, Carl J Lavie C et al. β-Blockers in hypertension, diabetes, heart failure and acute myocardial infarction: a review of the literature. Open Heart. 2015; 2(1): e000230.
4) Akbar S, Alorainy MS. The current status of beta blockers’ use in the management of hypertension. Saudi Med J. 2014; 35(11):1307-1317.
5)https://www.medicinenet.com/beta_blockers/article.htm#which_drugs_and_supplements_interact_with_beta_blockers
6) Pharmacology and pharmacotherapeutics. 24th edition.
Thanks for share knowledge
You are welcome. Please, keep visiting our website.