- ACE (Angiotensin Converting Enzyme) inhibitors or ACE-I are among the most widely used cardiovascular medicines. Their introduction in 1980s improve the management of hypertension.
- Captopril was the first ACE inhibitor introduced in 1981. Some other examples of ACE inhibitors are:
- Ramipril
- Enalapril
- Fosinopril
- Quinapril
- Benazepril
- Lisinopril
Mechanism of Action of ACE inhibitors
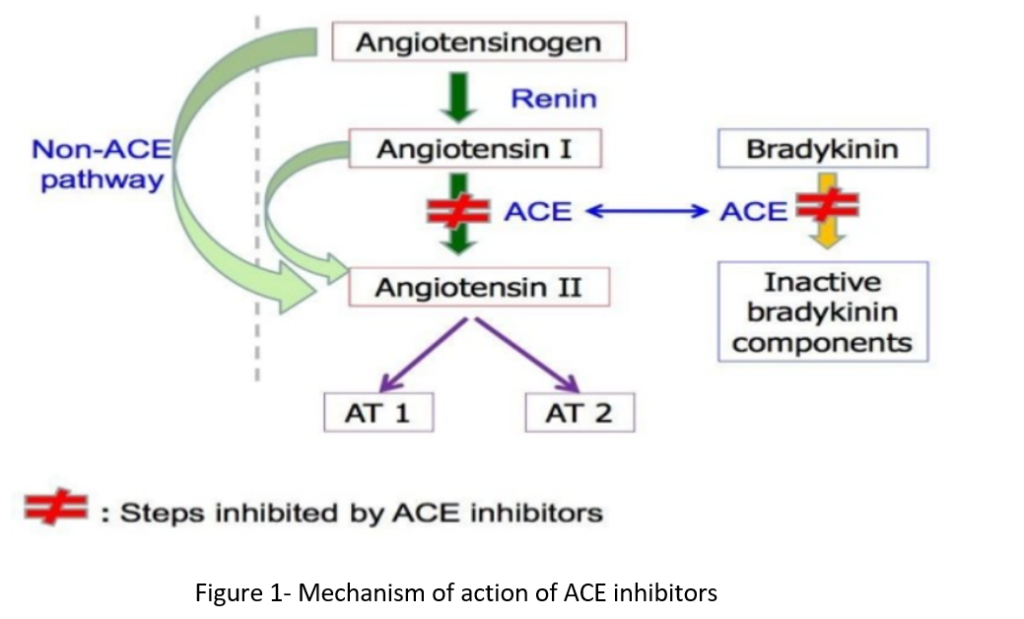
- ACE (angiotensin converting enzyme) cleaves inactive angiotensin I to active angiotensin II which is a potent vasoconstrictor. It is also involved in breakdown of bradykinin, a peptide that increases production of nitric oxide and prostacyclin, both of which are potent vasodilators.
- ACE inhibitors competitively inhibit ACE and inhibit conversion of angiotensin I to angiotensin II. It results in prevention of:
- Pressor effect of angiotensin II.
- Stimulation of aldosterone synthesis and release resulting in decreased sodium and water retention.
- Metabolism of bradykinin by ACE.
- Thus, vasodilation of both arterioles and veins occur as a result of decreased vasoconstriction (due to decreased angiotensin II) and enhanced vasodilation (due to increased bradykinin).
Pharmacokinetics of ACE inhibitors
- All the ACE inhibitors are available in oral formulation. Most of ACE inhibitors except captopril and lisinopril are prodrug which require conversion to active metabolites (e.g. Enalapril to enalaprilat).
- Enalaprilat is the only ACE inhibitor which is available intravenously.
- They differ in their pharmacokinetic parameters. Most of them have long half-life which allows once a day dosing except captopril.
| Drug | t1/2 (in hours) |
| Captopril | 1.9 |
| Lisinopril | 11-12 |
| Enalapril | 11-12 |
| Ramipril | 13-17 |
| Benazepril | 10-11 |
| Fosinopril | 12 |
| Quinapril | 3 |
Table 1- ACE inhibitors and their half-lives
- All drugs except captopril and lisinopril undergo hepatic conversion to active metabolites, so these two agents are preferred in patients with hepatic impairment.
- Most of them are excreted by kidney in the form of urine. Fosinopril is not excreted by kidney so doesn’t require dose adjustment in renal patients.
Therapeutic Uses
- Used as first- or second-line agents in hypertension. They are used alone or in combination with other drugs.
- For symptomatic treatment of chronic heart failure.
- Used in patients with diabetic nephropathy as they slow its progression and decrease albuminuria.
- It is used in patients at increased risk pf coronary artery disease.
- Used to reduce risk of heart attack and risk in ischemic heart disease.
Adverse Effects
- Most common adverse effect is persistent dry cough which occur in 5-30 % of cases. It is due to increased bradykinin. It is often mild but may be troublesome. Other common adverse effects include rash, fever, muscle cramp, GI disturbances and altered taste.
- First dose hypotension may occur in people with severe hypertension who are on multidrug therapy including diuretics. In such cases, it should be started in very small dose and preferably after stopping diuretics.
- Hyperkalemia may occur (particularly in patients with renal insufficiency) so potassium level should be continuously monitored.
- Angioedema is rare but potentially life-threatening condition.
- Functional renal failure in patients with severe bilateral renal artery stenosis.
Contraindication
- ACE inhibitors are contraindicated in pregnancy as they cause fetal malformation.
- They are contraindicated in patients with severe bilateral renal artery stenosis, aortic stenosis and coarctation of the aorta.
Use in COVID-19 infection
- There are two types of ACE enzyme; ACE-1 and ACE-2. It is known that ACE-2 acts as functional receptor for coronaviruses including SARS-CoV-2.
- Since ACE inhibitors inhibit ACE-1 activity and increase ACE-2 activity substantially over one to two weeks, many people were worried that ACE inhibitors may increase susceptibility to the virus and severity of disease.
- However, there is no appropriate evidence that endorse change or avoidance of ACE-inhibitors for managing hypertension in the context of COVID-19 infection.
- According to American College of Cardiology, patients should continue taking these drugs for heart failure, hypertension or IHD and if COVID-19 infection occurs, individualized treatment decisions should be made based on patient’s hemodynamic status and clinical presentation.
References
- Momoniat T, Ilyas D, Bhandari S. ACE inhibitors and ARBs: Managing potassium and renal function. Cleveland Clinic Journal of Medicine. 2019; 86 (9): 601-607.
- Sanchis-Gomar, F. et al. Angiotensin-Converting Enzyme 2 and Anti-Hypertensives (Angiotensin Receptor Blockers and Angiotensin-Converting Enzyme Inhibitors) in Coronavirus Disease 2019 (COVID-19). Mayo Clinic Proceedings. 2020; 95 (6).
- Aronson JK, Ferner RE. Drugs and the renin-angiotensin system in covid-19. BMJ. 2020; 369.
- https://pharmafactz.com/ace-inhibitors-pharmacology/
- A textbook of clinical pharmacology and therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- Pharmacology and pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.