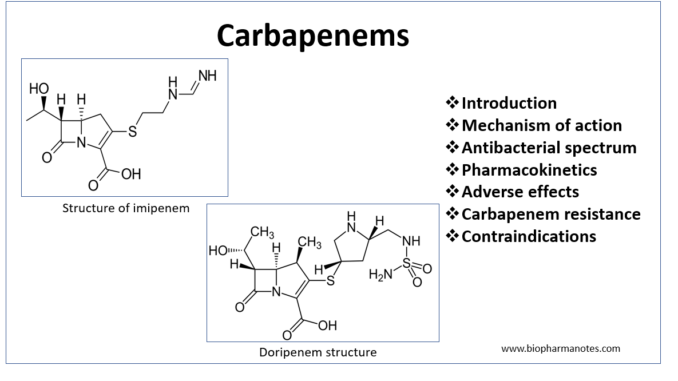
- Carbapenems are beta- lactam antibiotics which have broader spectrum of activity and great potency compared to other beta-lactam antibiotics. They are closely related to penicillin. The slight difference in structure is sulfur atom of thiazolidine ring of penicillin is externalized and replaced by a carbon atom in carbapenem. This carbon is responsible for carbapenem’s potency, spectrum of activity and stability against β-lactamase.
- The first carbapenem to be discovered is thienamycin which is obtained from Streptomyces cattleya. It is considered as lead compound of carbapenem. All other carbapenems are synthetic derivatives of thienamycin.
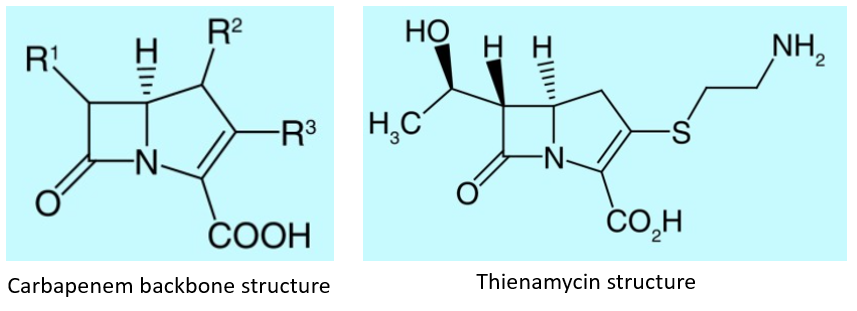
Figure Source- Ann et al, 2020.
- Some commonly used examples of carbapenems are:
- Imipenem
- Meropenem
- Doripenem
- Faropenem
Mechanism of action of carbapenems
- The mechanism of action is similar to penicillin. They penetrate bacterial cell wall and bind to enzymes known as penicillin binding proteins (PBPs) which are located on cell membrane. Transpeptidase is one of the PBP involved in synthesis of peptidoglycans. Binding of carbapenem to transpeptidase inhibits synthesis of peptidoglycans which leads to weakening of bacterial cell wall.
- Hence, the bacteria become vulnerable to rupture by solutes in surrounding medium. Carbapenems are resistant to hydrolysis by most of the beta-lactamases.
Anti-bacterial spectrum of carbapenems
- They have wider spectrum of antibacterial activity compared to penicillin, cephalosporin and beta-lactam/beta-lactamase inhibitor combination.
- Imipenem is active against beta-lactamase producing gram-positive and gram- negative bacteria, anaerobes. Meropenem and doripenem has similar antibacterial spectrum as of imipenem. Meropenem, biapenem, diripenem and ertapenem are slightly more active against gram negative organism. Ertapenem, unlike other carbapenems, is not active against Enterococcus species, P. aeruginosa and Acinetobacter species.
- Meropenem is less potent than imipenem or doripenem against P. aeruginosa.
- Carbapenems are effective against enterococci except Enterococcus fecium. They are active against MRSA and non- beta lactamase producing penicillin resistant strains.
Indications of carbapenems
- Used for wide variety of infection like urinary tract, gynecological, lower respiratory tract and intra- abdominal infections.
- Also used in skin, bone, soft tissue and joint infection.
- Entrapenem is first choice of drug for monotherapy of serious, complicated, community acquired intrabdominal infections. Imipenem, doripenem and meropenem are used in high risk nosocomial and community acquired abdominal infections.
Pharmacokinetics
- Imipenem is administered with cilastatin to achieve prolonged half-life by inhibiting its renal metabolism. Other carbapenems don’t require administration with cilastatin.
- Imipenem/ cilastatin and meropenem are administered via IV route. Ertapenem can be administered through IV or IM route. Half-life may vary. For imipenem, meropenem and doripenem, in- vivo half-life is around 1 hour. Half-life of ertapenem is around 4 hours so it is administered once a day. They penetrate in most of the body tissues and fluids. They can also penetrate CSF (cerebrospinal fluid) when meninges are inflamed. Meropenem can penetrate CSF even in absence of inflammation.
- Among all carbapenems, doripenem is least susceptible to hydrolysis by carbapenemases. Its hydrolysis is 2-150 times slower than of imipenem.
Adverse effects
- The most common side effect is nausea and vomiting. When used in high doses, can induce seizure (1.5 % of patients). Chances of seizure is high with imipenem.
- Imipenem can cause pseudomembranous colitis and transient elevation of liver enzymes in blood.
Carbapenem resistance
- Carbapenem resistance is current ongoing major health problem. Resistance to carbapenem may develop due to intrinsic or acquired resistance mechanism or both. The acquired mechanism to develop resistance to carbapenem include- porin mediated resistance to reduce uptake of carbapenem, efflux pump which pump carbapenem out of the cell and enzyme mediated resistance via carbapenemase genes.
- Enzyme mediated resistance is most common. It is due to production of β-lactamases (carbapenemases) which are capable of hydrolyzing carbapenems and other β-lactam antibiotics. Carbapenemase can inactivate most of β- lactams and are encoded by genes carried on transposons, plasmids or other mobile genetic elements which can even be transferred to other bacterial species. Hence, it is of greatest threat.
Contraindications
- Contraindicated in patients allergic to β-lactam antibiotics.
- Contraindicated in epileptic patients who are on valproic acid therapy as they decrease concentration of valproic acid.
References
- Codjoe et al. Carbapenem Resistance: A Review. Med Sci (Basel). 2018 Mar; 6(1): 1.
- Ann et al. A review on bacterial resistance to carbapenems: epidemiology, detection and treatment options. Future Sci OA. 2020; 6(3): FSO438.
- Krisztina et al. Carbapenems: Past, Present, and Future. Antimicrobial agents and chemotherapy. 2011; 55(11): 4943–4960.
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- https://www.ncbi.nlm.nih.gov/books/NBK551704/