- Metformin is a biguanide, a drug class of herbal origin that has been widely used to treat diabetes since 1950s. It is the only biguanide currently used. It was initially extracted from the plant Galega officinalis (French lilac). Chemically, it is 1,1-dimethylbiguanide hydrochloride.
- It was discovered in 1922, was introduced in medical market of France in 1957 and in USA in 1995. It is included in World Health Organization’s (WHO) List of essential Medicines.
- According to American Diabetes Association (ADA) Guidelines, metformin is most recommended and commonly prescribed among all anti-diabetic drugs for type 2 diabetes. It was fourth most commonly prescribed medicines in United States in 2017.
Mechanism of action of metformin
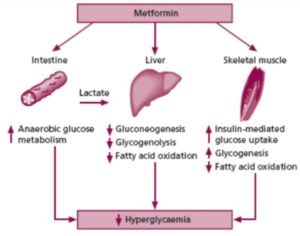
Figure- Mechanism of action of Metformin (Source-Br J Diabetes Vasc Dis, 2006)
- The mechanism of metformin is not completely understood. It is classified as insulin sensitizer.
- Several mechanisms involved in anti-diabetic activity of metformin are:
- Inhibition of hepatic neoglucogenesis and decreases hepatic and renal glucose output. (Very major role in anti-diabetic activity)
- It increases peripheral glucose utilization by enhancing anaerobic glycolysis.
- It delays glucose absorption.
- Acts as insulin sensitizer in the muscle and adipose tissue and reduces hyperinsulinemia. (very minor role)
- It reduces the appetite which is useful in obese diabetic patients.
- It doesn’t stimulate insulin release from pancreatic beta cells. So, the risk of hypoglycemia is less than that of sulfonylurea.
Pharmacological actions of metformin
- It doesn’t decrease blood sugar level in normal person.
- It potentiates hypoglycemic action of insulin and sulfonylurea and reduces plasma total and LDL (Low density lipoprotein) cholesterol and triglyceride level. Metformin increases plasma fibrinolytic activity and reduce lipolysis, FFA production and lipid oxidation.
- Metformin doesn’t inhibit ketogenesis in liver. It decreases glycogen content of the liver.
- It may cause weight loss due to reduction in appetite. Hence, it is beneficial to prevent weight gain compared to sulfonylurea.
Pharmacokinetics of metformin
- Metformin belongs to class of oral anti-diabetic agents. It undergoes rapid absorption from small intestine. Presence of food slightly delays its absorption.
- Available as tablet, solution, extended release tablet or extended release suspension.
- It is stable, doesn’t bind to plasma proteins, doesn’t undergo hepatic metabolism (no metabolites have been identified in human) and biliary excretion. Excretion takes place via urine (most in unchanged form).
- Half-life is 1.5-4 hours. It is widely distributed in body tissues including intestine, liver and kidney.
- The maximum recommended daily dose of metformin is 2.5 gm divided into three doses with meals.
Therapeutic Uses
- Used as first-line pharmacologic treatment for type 2 diabetes which cannot be controlled by diet alone. Used alone or in combination with insulin or other glucose lowering therapies.
- In obese patients with type 2 diabetes mellitus.
- In secondary sulfonylurea failure.
- To treat polycystic ovary syndrome (PCOS).
Adverse Effects
- It is generally well tolerated.
- Acute side effects occur in about 20% of patients and includes gastrointestinal side effects like bitter or metallic taste, nausea, diarrhea, abdominal discomfort and anorexia. These can be minimized by increasing the dose of metformin gradually and taking it with meals.
- Long term use may interfere with vitamin B-12 and folate absorption.
- Lactic acidosis, which occur rarely, could be lethal.
Drug Interaction
- Cimetidine (H2 receptor antagonist) decrease clearance of metformin by kidneys and increase its plasma concentration.
- It may interact with anti-cholinergic medications.
- Taking it with drugs like acetazolamide, methazolamide, topiramate, zonisamide may increase risk of lactic acidosis.
Contraindication
- It is contraindicated in patients with history of lactic acidosis, in renal dysfunction (due to risk of lactic acidosis).
- Contraindicated in hepatic disease, chronic hypoxic lung disease or cardiac failure requiring drug therapy, acute myocardial infarction, exacerbation of heart failure or sepsis. These conditions predispose to fatal complication of lactic acidosis.
- Should be used with caution in older patients (˃ 80 years), in those with heart failure or alcohol abuse.
- It should be temporarily discontinued in patients undergoing radiocontrast study (CT scan or coronary angiography). It should be stopped one day before and for 48 hours after the procedure.
References
- Flory J, Lipska K. Metformin in 2019. JAMA. 2019; 329(19): 1926-1927.
- Dumitrescu R, Mehedintu C, Briceag I, Purcarea VL, Hudita D. Metformin-Clinical Pharmacology in PCOs. J Med Life. 2015; 8(2): 187–192.
- Foretz M, Guigas B, Viollet B. Understanding the glucoregulatory mechanisms of metformin in type 2 diabetes mellitus. Nature Reviews Endocrinology. 2019; 15: 569–589.
- Zhou J, Massey S, story D, Li L. I Metformin: An Old Drug with New Applications. Int J Mol Sci. 2018; 19(10): 2863.
- https://en.wikipedia.org/wiki/Metformin
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.