- Clindamycin is lincosamide antibiotic. It is 7(S)- chloro-7- deoxylincomycin, a semisynthetic derivative of lincomycin which is a natural antibiotic produced by actinobacterium Streptomyces lincolnesis.
- It has replaced lincomycin due to its improved properties over its parent compound.
Indications of clindamycin
- To treat Gram +ve organism resistant to penicillin or cephalosporin.
- To treat serious anaerobic infections. For this, it is used in combination with aminoglycosides.
- Used to treat staphylococcal bone and joint infection, actinomycosis, anthrax and diphtheria.
- Used in treatment of septicemia, intra-abdominal infections and lower respiratory tract infection.
- It is used topically in treatment of acne vulgaris.
- Available as vaginal cream or suppository for treating bacterial vaginosis in non-pregnant female.
- It has some activity against protozoans. Hence used in combination with other drugs to treat malaria and toxoplasmosis.
- Used for prophylactic treatment against Viridans group streptococcal infection in patients undergoing oral, dental or upper respiratory surgery. Also used for prophylaxis against bacterial endocarditis in penicillin allergic patients.
Antibacterial spectrum of clindamycin
- It acts as bacteriostatic at low concentration and bactericidal at slightly higher concentration. Clindamycin is most active against aerobic gram-positive cocci and bacilli including streptococci, pneumococci, staphylococci. It is effective against methicillin resistant Staphylococcus aureus.
- Effectiveness of clindamycin against anaerobic bacteria is high compared to erythromycin or clarithromycin. It is not effective against aerobic gram- negative bacilli.
Resistance
- Resistance to clindamycin has been increasing which is limiting its use. Resistance may occur due to multiple reasons including:
- The presence of efflux pump.
- Chromosomal mutation that alter 50S ribosomal protein.
- Ribosomal protection by inducible or constitutive production of methylase enzymes that modify ribosomal target and decrease drug binding.
- Hydrolysis of erythromycin by esterase produced by gram-negative organisms such as Enterobacteriaceae.
- The inability of organism to take up the antibiotic.
Mechanism of action of clindamycin
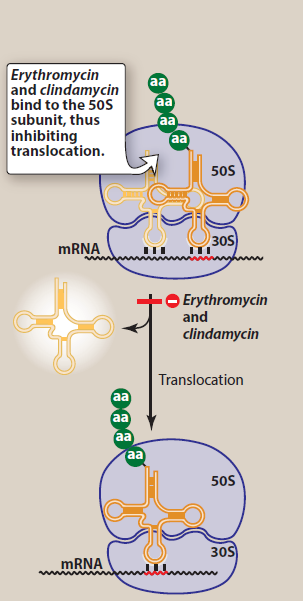
Figure- Mechanism of action of clindamycin (Source- Lippincott’s Illustrated Reviews)
- Its mechanism of action is similar to that of erythromycin. It acts as a protein synthesis inhibitor. It binds to 23S RNA of 50S ribosomal subunit of bacteria and inhibits protein synthesis by inhibiting translocation step.
- The binding sites of clindamycin, erythromycin and chloramphenicol are in close proximity.
Pharmacokinetics
- It is administered through various routes including oral, IM, IV, topical route in the form of gel, foam, lotion or solution. It is available as cream or suppository for intravaginal administration. When administered through oral route, it is taken with full glass of water to minimize esophageal ulceration. It’s absorption is not affected by presence of food.
- It is highly protein bound and is distributed in all body fluids and tissues including bone and joints. It shows poor penetration into CNS, however concentration sufficient to treat cerebral toxoplasmosis is achieved.
- Metabolism takes place in liver. It undergoes oxidative metabolism to inactive products and is mainly excreted via bile. Dose modifications are required in patients with hepatic failure and concomitant renal or hepatic dysfunction.
Adverse effects
- Diarrhea is most common adverse effect which is due to pseudomembranous colitis cause by overgrowth of C. difficile. C. difficile toxins may cause abdominal pain, fever and bloody diarrhea which is highly lethal and can be treated using oral metronidazole or vancomycin.
- It can cause rashes in around 10% of patients. It is more common in HIV infected patients. Some other rare side effects are thrombocytopenia, granulocytopenia, local thrombophlebitis and reversible elevation of serum transaminases.
Drug Interactions
- As ribosomal binding site of clindamycin, erythromycin and chloramphenicol are in closer proximity, these three drugs may exhibit mutual antagonism.
- It causes slight potentiation of action of neuromuscular blockers.
Contraindications
- Contraindicated in patients with history of pseudomembranous colitis or ulcerative colitis.
- Contraindicated in patients with hypersensitivity to clindamycin, lincomycin or their components.
References
- https://www.ncbi.nlm.nih.gov/books/NBK519574/
- https://go.drugbank.com/drugs/DB01190
- Smieja M. Current indications for the use of clindamycin: A critical review. Can J Infect Dis. 1998; 9(1): 22–28.
- Pharmacology and Pharmacotherapeutics book. 24th edition.
- Goodman and Gillman’s Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology. 6th edition.
- A Textbook of Clinical Pharmacology and Therapeutics. 5th edition.