- Albendazole is broad spectrum anthelminthic agent used to treat various parasitic worm infection. It is also known as albendazolum.
- It belongs to benzimidazole group and is synthetic nitroimidazole. Other commonly used benzimidazole are mebendazole and thiabendazole.
- It was developed in 1975, introduced as anthelminthic agent for sheep in 1977. It was introduced for human use in 1982. Albendazole is included in World Health Organization’s List of Essential Medicines.
Mechanism of action of Albendazole
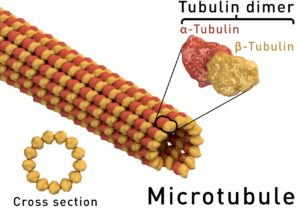
Figure – A microtubule is composed of polymer of α and β tubulin
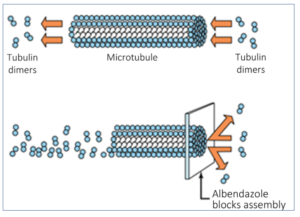
Figure 2- Mechanism of action of albendazole
- It has multidimensional mechanism of action including following;
Inhibits beta-tubulin– inhibit both polymerization and formation of microtubules. Affinity of albendazole binding to beta-tubulin of microbe is higher than of mammalian protein.
Inhibits cell division– by preventing formation of spindles.
Glycogen depletion– it decreases glucose uptake in both larval and adult parasites.
Motility disruption– it alters cell motility and intracellular transport mechanisms.
- It is active against both larva and adult stages of nematodes and has ovicidal action against ascariasis, Trichuris and ancylostomiasis.
Pharmacokinetics of Albendazole
- It can be administered orally in the form of suspension, granules, tablets, pastes or as bolus preparation. After oral administration, it is absorbed rapidly. Its absorption is increased by high-fat meal.
- After absorption, it undergoes hepatic 1st pass metabolism to active metabolite, albendazole sulfoxide. The formation of albendazole sulfoxide is catalyzed by both microsomal flavin monooxygenase and CYP isoforms in the liver. Around 70% of albendazole sulfoxide bind to plasma proteins. It has variable half-life of around 4-15 hours.
- It is well distributed into various tissues including bile, cerebrospinal fluid (CSF) and hydatid cyst. Albendazole metabolites are excreted mainly though urine.
Therapeutic Uses of Albendazole
- Ascariasis, ancylostomiasis and trichuriasis: Usually 400 mg single dose for adults and children above 2 years age. In children between ages of 12- 24 months, less than 200 mg is recommended. Hookworm and trichuriasis may need a repeat dose.
- Enterobiasis: 400 mg single dose, repeated after 4 weeks.
- Hydatid disease: 400 mg bid with meal for one month or longer.
- Strongyloidiasis: 400 mg twice daily for 3 days, repeated after 3 weeks if necessary.
- Trichinella spiralis: 400 mg bid for 8-14 days.
- Cysticercosis: It is considered because of short course, less toxicity than praziquantel, better penetration into CSF and cost. It is given 400 mg bid for 21 days. For children, the dose is 15mg/kg/day (maximum 800 mg). A glucocorticoid is started prior to albendazole to decrease inflammatory reaction caused by dead parasites.
- It is included in programs to control lymphatic filariasis. Mostly, it is used in combination with either diethylcarbamazine or ivermectin.
- It is effective for therapy of microsporidial intestinal infection in AIDS patients.
- For treating ocular toxocariasis in combination with systemic steroids.
- It is also used as veterinary medicine.
Adverse Effects
- When used for short duration (1-3 days), it is well tolerated and is nearly free from significant side effects. Mild and transient GI upset, diarrhea, headache, nausea, dizziness and fatigue. Allergic reaction is rare and may resolve after 48 hours.
- When used for long term therapy as in hydatid disease, it is well tolerated but can cause some side effects. The side effects include abdominal distress, severe headache, alopecia, fever, leucopenia and thrombocytopenia.
- During long term therapy, increase in liver enzymes or serum transaminoferases is common, which return to normal after drug cessation. Jaundice or cholestasis may occur rarely. Liver function and blood count of patient on long term therapy should be monitored.
- If patients are not pretreated with glucocorticoids during neurocysticercosis, they may experience serious neurological sequalae.
Drug Interaction
- Concurrent administration of glucocorticoids and praziquantel increase plasma level of sulfoxide metabolite.
- When used together with hepatic CYP inhibitors, caution is advised.
Contraindication
- It should not be given to patients with known hypersensitivity to benzimidazole drugs.
- It belongs to category C drugs which means its safety in pregnancy is not established. So, it is recommended to avoid its use in first trimester of pregnancy and should be avoided upto 1 month before conception.
- It is not used in patient with liver cirrhosis.
References
- https://www.brainkart.com/article/Albendazole_25095/
- https://www.researchgate.net/publication/11951935_Albendazole_A_review_of_anthelmintic_efficacy_and_safety_in_humans
- Csiko GY, Banhidi GY, Semjen G, Laczay P, Sandor GV, Lehel J et al. Metabolism and pharmacokinetics of albendazole after oral administration to chickens. vet. Pharmacol. Therap. 1996; 19; 322-325.
- Steiger U, Cotting J, reichen J. Albendazole treatment of echinococcosis in humans: Effects on microsomal metabolism and drug tolerance. Clinical Pharmacology and Therapeutics. 1990; 47: 347–353.
- Asenbauer TB, Maca SM, Hauff W, Kaminski SL, Domanovits H, Theyer I etal. Treatment of Ocular Toxocariasis with Albendazole. Journal of Ocular Pharmacology and Therapeutics. 17, No. 3 .
- Radko L, Minta M, Jedziniak P, Treba SS. J Comparison of Albendazole Cytotoxicity in Terms of Metabolite Formation in Four Model Systems. Vet Res. 2017; 61(3): 313–319.
- Principles and Practice of Pediatric Infectious Diseases (Fourth Edition). Part IV, 2012; 1518-1545. e3.
- Pharmacology and Pharmacotherapeutics book. 24th edition.
- Goodman and Gillman’s Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology. 6th edition.