Peptic Ulcer
- Ulcers are deep lesions penetrating through the entire thickness of the gastrointestinal tract mucosa and muscularis mucosa. Peptic ulcer is one of the common GI disorders. Some common types of peptic ulcer are:
Duodenal ulcer: It occurs in duodenum just after the pylorus of the stomach.
Gastric ulcer: It occurs in stomach particularly in lower half portion.
Table 1- Differences between gastric and duodenal ulcer
| Duodenal Ulcer | Gastric Ulcer |
| Pain relieved by meal | Pain increased by meal |
| Occurs 2-3 after meal | Occurs 30 minutes- 1 hour after meal |
| Most common type | Not so common |
| Dark, tarry stool occurs | Vomiting occurs |
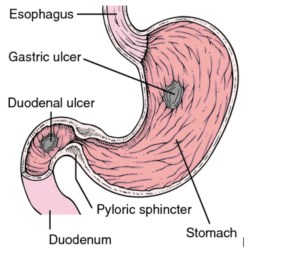
Figure 1- Occurrence of gastric and duodenal ulcer (Source- The Free Dictionary by Farlex)
About two third of patients with peptic ulcer disease are found to be asymptomatic. In symptomatic patients, the most common symptoms include:
- Abdominal pain and discomfort
- Weight loss
- Poor appetite
- Nausea and vomiting
- Some may experience blood in stool and vomit and black stool which indicate gastrointestinal bleeding
Etiology and Pathogenesis of peptic ulcer
1) Helicobacter Pylori (H. Pylori)
- It is the main cause of stomach ulcers. H. Pylori is a gram-negative bacillus, motile, flagellated, microaerophilic and spiral shaped bacteria. It was first noticed by a pathologist, Dr. Warren as “numerous curved bacilli lying below the stomach’s protective mucus in a gastric biopsy sample” (1979). Later, Warren and Marshall conclusively showed the association of these bacilli, now known as Helicobacter pylori, with chronic gastritis and ulceration. They were awarded the Nobel Prize for this in 2005.
- The method of H. Pylori transmission is unclear. It seems to be spread from person to person via faeco-oral route. It secretes two important things: urease which hydrolyze urea into carbon dioxide and ammonia and ammonia helps it to survive in acidic environment of stomach, an exotoxin which directly damages the epithelial cells.
- H. Pylori infection may also reduce somatostatin content and increase gastric secretion by causing hypergastrinemia leading to increase in histamine secretion and finally increased secretion of acid or pepsin form parietal cells. Nearly all patients with duodenal ulcer and 80% of the patients with gastric ulcer show colonization of stomach by H. Pylori. They are also involved in pathogenesis of gastric carcinoma and gastric lymphoma.
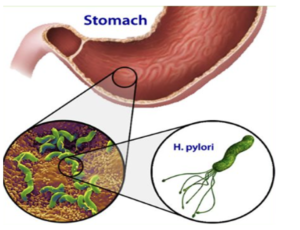
Figure- H. pylori induced ulcer
2) Gastric acid secretions:
- It is one of the major ulcerogenic factor responsible for inducing gastric ulcer. About 50 % of gastric ulcer patients are pepsin and acid hyper secretors. It also plays an important role in mucosal defense to prevent entry and colonization of bacteria in mucosal layer.
- Gastric juice is a mixture of HCl, pepsin, mucus, neutral chlorides, intrinsic factor and traces of potassium, ammonium and calcium. Gastric acid and pepsin are secreted by parietal cells which are in the walls of the midsection of the oxyntic glands, the secretory unit of gastric mucosa. Secretion of gastric acid is regulated by central and peripheral mechanism. The parietal cell possesses specific hydrogen-potassium-ATPase enzyme (proton pump) which is common final pathway for gastric acid secretion. It is activated by protein kinases, histamine, acetylcholine and gastrin. When activated, H+ ions are transported in exchange of K+ ions. The H+ ions then combine with Cl– ions to form HCl.
Acid secretion from parietal cells is regulated by three distinct but interdependent pathways:
The neurocrine pathway
- which acts through vagal efferent transmitter, acetylcholine.
The endocrine pathway
- which delivers hormone gastrin from antral G cells.
The paracrine pathway
- which delivers histamine from ECL (Enterochromaffin like cells).

Figure 2- Mechanism involved in regulation of gastric acid secretion by parietal cells (M1 – Muscarinic, H2– Histaminic, R- Receptor, Ach- Acetylcholine, EP-R- Prostaglandin receptor for PGE2) (Source- Pharmacology and Pharmacotherapeutics 24th edition)
- Surface of parietal cell has receptors like H2receptor which responds to histamine released from mast cells, receptor responsive to gastrin and receptor responsive to muscarinic effects of acetylcholine released from the vagus nerve. Gastrin stimulate acid secretion either by directly stimulating parietal cells or by stimulating release of histamine from ECL. The muscarinic 1 agonist stimulate acid secretion by direct action on muscarinic receptor and also by stimulating histamine secretion.
3) NSAIDs (Non- Steroidal Anti-Inflammatory Drugs):
- NSAIDs like aspirin, paracetamol are a broad class of non-glucocorticoid drugs which are used as anti-inflammatory, analgesic and anti-pyretic agents. About 25 % of chronic users of NSAIDs develop gastric ulcer disease.
- These drugs inhibit COX- 1 and COX-2 (Cyclooxygenase) enzymes which convert arachidonic acid (AA) to prostaglandin (PGs). This inhibition leads to impairment of mucosal barrier causing corrosive action with pepsin and resulting in progression of peptic ulcer. Inhibition of COX-1 enzyme cause release of the endothelin-1 which induce mucosal injury by contraction of blood vessels. NSAIDs also causes reduction in mucosal blood flow, mucosal bicarbonate secretions, impaired platelet aggregation and increased leucocyte adherence which are involved in pathogenesis of ulceration.
- Risk factors related to NSAIDs induced peptic ulcer are H. Pylori infection, previous history of GI ulcer, high dose of NSAIDs, multiple drug combination therapy and comorbidities like cardiovascular diseases and nephropathy.
-
4) Stress:
- Psychological stress acts as cofactor along with H. Pylori in pathogenesis of peptic ulcer. It may act by stimulating the production of gastric acid or by promoting behavior that causes risk to health.
-
5) Zollinger- Ellison syndrome
It is a rare condition in which tumors are formed in pancreas or duodenum and secrete large amount if hormone gastrin which ultimately lead to increased gastric acid production causing ulcer. This disease may occur at any time in life.
References
- Lucija Kuna, Jelena Jakab, Robert Smolic, Nikola Raguz-Lucic, Aleksandar Vcev, and Martina Smolic. Peptic Ulcer Disease: A Brief Review of Conventional Therapy and Herbal Treatment Options. J Clin Med. 2019 Feb; 8(2): 179.
- Susan Levenstein, adjunct research physician. Stress and peptic ulcer: life beyond helicobacter. BMJ 1998; 316.
- V Prabhu and A Shivani. An Overview of History, Pathogenesis and Treatment of Perforated Peptic Ulcer Disease with Evaluation of Prognostic Scoring in Adults. Ann Med Health Sci Res. 2014 Jan-Feb; 4(1): 22–29.
- Majumdar D, Bebb J, Atherton J. Helicobacter pylori infection and peptic ulcers. Med 2011:39;154-161.
- Ludovico B, Eric S, Annemarthe G. Van DV, Ri no R, Antonello C. Helicobacter Pylori cytotoxin-associated gene A subverts the apoptosis-stimating protein of p53 ASPP2 tumor suppressor pathway of the host. 2011; 1-6.
- Martin JB. Not all Helicobacter pylori strains are created equal; should all be eliminated. Lancet 1997; 349: 1020-22
- Vane JR, Botting RM. Mechanism of action of non-steroidal anti-inflammatory drugs. Am J Med 1998: 104; 2S-8S.
- Whittle BJ. Gastrointestinal effects of nonsteroidal anti-inflammatory drugs. Fundam Clin Pharmacol 2002; 17:301–313.
- Zhonghua Nei Ke Za Zhi. Recommendation for the prevention and treatment of non-steroidal anti-inflammatory drug-induced gastrointestinal ulcers and its complications. 2017 Jan 1;56(1):81-85.
- Pharmacology and pharmacotherapeutics. Page no- 633-637.
- Goodman and Gillman Manual of Pharmacology and Therapeutics. Page no- 631-632.
- A textbook of clinical pharmacology and therapeutics. Page no- 247-248.