- Erythromycin is an antibiotic used to treat various bacterial infections. It is derived from the fungus Streptomyces erythreus.
- Erythromycin belongs to family of macrolide antibiotics (the name macrolide is due to presence of large lactone ring in their chemical structure). It is first macrolide antibiotic to be approved for clinical use in 1950s. The other members of this group are azithromycin, oleandomycin, spiramycin and clarithromycin.
- It is available both as generic and brand medicine. It is included in World Health Organization’s List of Essential Medicines.
Mechanism of action of erythromycin
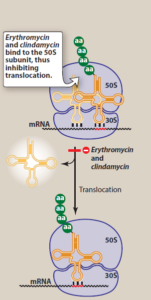
Figure 1- Mechanism of action of Erythromycin (Source- Lippincott’s Illustrated Reviews)
- It acts as a protein synthesis inhibitor. It binds to 50S ribosomal subunit of bacteria and inhibits protein synthesis by inhibiting translocation step. The binding site is either same or very near to binding site of clindamycin and chloramphenicol. It also affects other steps like transpeptidation.
- Depending on its concentration, it acts either as bacteriostatic or bactericidal.
Antibacterial spectrum of erythromycin
- It is most active against aerobic gram-positive cocci and bacilli including streptococci, pneumococci, staphylococci.
- It is inactive against most aerobic enteric gram-negative bacilli. However, it has mild activity against other gram-negative organisms including influenzae and N. meningitidis and is active against N. gonorrhoeae. It is also active against Borellia spp, Bordetella pertussis and Pasteurella multocida.
Resistance
- Resistance to erythromycin has been increasing which is limiting its use. Resistance may occur due to multiple reasons including:
- The presence of efflux pump.
- Chromosomal mutation that alter 50S ribosomal protein.
- Ribosomal protection by inducible or constitutive production of methylase enzymes that modify ribosomal target and decrease drug binding.
- Hydrolysis of erythromycin by esterase produced by gram-negative organisms such as Enterobacteriaceae.
- The inability of organism to take up the antibiotic.
Indications of erythromycin
- In patients allergic to penicillin or who have developed penicillin resistance.
- It is the drug of choice in mycoplasma (mycoplasma pneumoniae) and chlamydial infections.
- Drug of choice in whopping cough caused by pertussis and diarrhea caused by Campylobacter jejuni.
- In legionnaires disease caused by legionella.
- Effective alternative as prophylactic agent for recurrence of rheumatic fever in patients allergic to penicillin.
- In STDs like syphilis, chancroid.
- Used for treating acne in combination with benzoyl peroxide.
Pharmacokinetics
- Erythromycin base is destroyed by gastric acid, so it is used in form of enteric coated tablets or esterified form (stearate, estolate, ethylsuccinate) for oral administration. Food may impair absorption. IV administration can help to achieve higher concentration.
- It is distributed to all body fluids except in brain and CSF (Cerebrospinal Fluid). It can cross placenta and is also secreted in milk. Erythromycin can also diffuse into prostatic fluid and is accumulated in macrophages.
- It is extensively metabolized in liver, interacts with cytochrome P450 system and inhibits oxidation of several drugs.
- It is excreted in bile as active drugs. Some percentage of drug is excreted in urine as active drug (2-5% after oral administration and 12-15% after IV infusion). Hence, it isn’t routinely recommended to reduce dose in renal insufficiency.
- Peak plasma level is achieved within 2-4 hours after a single oral dose. The plasma half-life is around 1.6 hours.
Adverse effects
- Common side effects include nausea, vomiting, allergic reaction (fever, eosinophilia, urticaria, dermatitis, lymphadenopathy), diarrhea and epigastric pain. Gastric upset may lead to poor patient compliance.
- Higher dosage may lead to transient deafness. Erythromycin estolate may cause jaundice and cholestatic hepatitis which is resolved within few days of drug cessation.
- It can cause cardiac arrhythmia including QT prolongation with polymorphic ventricular tachycardia.
Drug Interactions
- It inhibits hepatic metabolism of several drugs and lead to accumulation and their toxic effects. These drugs include cimetidine, ketoconazole, carbamazepine, warfarin, cyclosporine, atorvastatin, simvastatin, theophylline, valproate and protease inhibitors.
Contraindications
- Contraindicated in patients who are allergic or hypersensitive to erythromycin or other macrolide antibiotics.
- Used with caution in patients with hepatic dysfunction.
- Used with caution in patients with pro-arrhythmic condition or who are using pro-arrhythmic agents.
References
- Hawkyard CV, Koerner RJ. The use of erythromycin as a gastrointestinal prokinetic agent in adult critical care: benefits versus risks. J Antimicrob Chemother. 2007; 59(3): 347-58.
- Shah F. Pediatrics in Review. April. 1998; 19 (4): 140-141.
- Curry JJ, Lander TD, Stringer MD. Erythromycin as a prokinetic agent in infants and children. Alimentary Pharmacology and Therapeutics. 2001; 15: 595-603.
- Pharmacology and Pharmacotherapeutics book. 24th edition.
- Goodman and Gillman’s Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology. 6th edition.
- https://www.ncbi.nlm.nih.gov/books/NBK532249/