
- Clarithromycin is a semi-synthetic macrolide antibiotic derived from erythromycin. It is similar to erythromycin in structure, except methylation of hydroxyl group in 6th position. Macrolide antibiotics are named so due to presence of large lactone ring in their chemical structure.
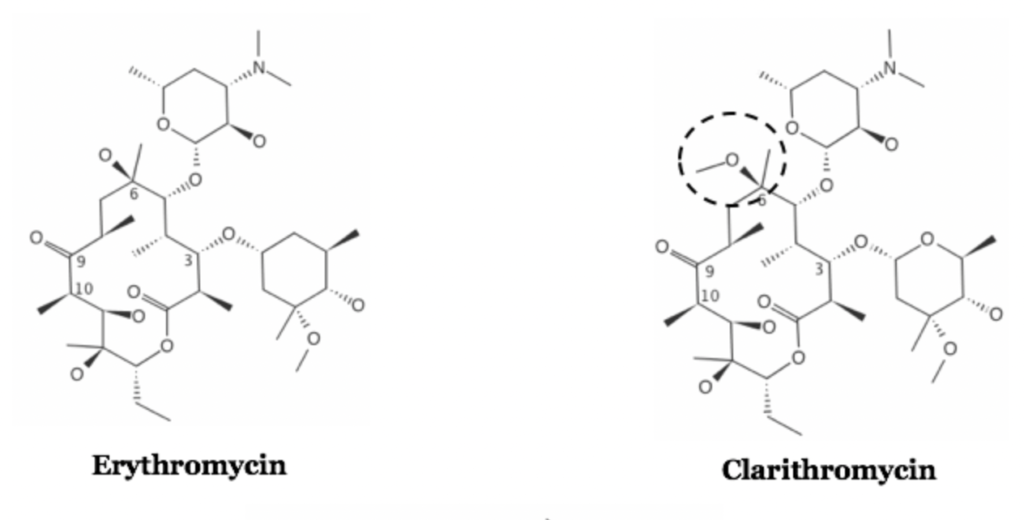
- Clarithromycin is chemically known as 6-O-methyl-erythromycin. Its activity is slightly greater than that of its parent compound, erythromycin. Clarithromycin is included in World Health Organization’s List of Essential Medicines.
Indications of clarithromycin
- For treating acute otitis media in patients hypersensitive to type I penicillin.
- For treating pharyngitis and tonsilitis.
- Used in respiratory tract infection including acute maxillary sinusitis, acute bacterial exacerbation of chronic bronchitis, Legionnaire’s disease, pertussis, and community acquired pneumoniae.
- In treatment of H. pylori infection, uncomplicated infection of skin and skin structure, bartonella infection, early Lyme disease. In H. pylori infection, it is used in combination as co-packaged triple therapy with amoxicillin and vonoprazan. It is effective than azithromycin against H. pylori and MAC (Mycobacterium Avium Complex).
- Also used in encephalitis caused by Toxoplasma gondi.
Antibacterial spectrum
- Clarithromycin has broad spectrum anti-microbial activity and is active against gram-positive, gram-negative bacteria, atypical pathogens, and some anaerobic bacteria. It is effective against aerobic gram-positive bacteria like S. aureus, S. pneumoniae and is also effective against aerobic gram-negative bacteria like H. influenzae and Moraxella catarrhalis.
- Also effective against H. pylori, mycobacteria, Mycoplasma pneumoniae and Chlamydia pneumoniae.
Resistance
- Resistance to clarithromycin may occur due to multiple reasons including:
- The presence of efflux pump.
- Chromosomal mutation that alters 50S ribosomal protein.
- Ribosomal protection by inducible or constitutive production of methylase enzymes that modify ribosomal target and decrease drug binding.
- The inability of organism to take up the antibiotic.
Mechanism of action of clarithromycin
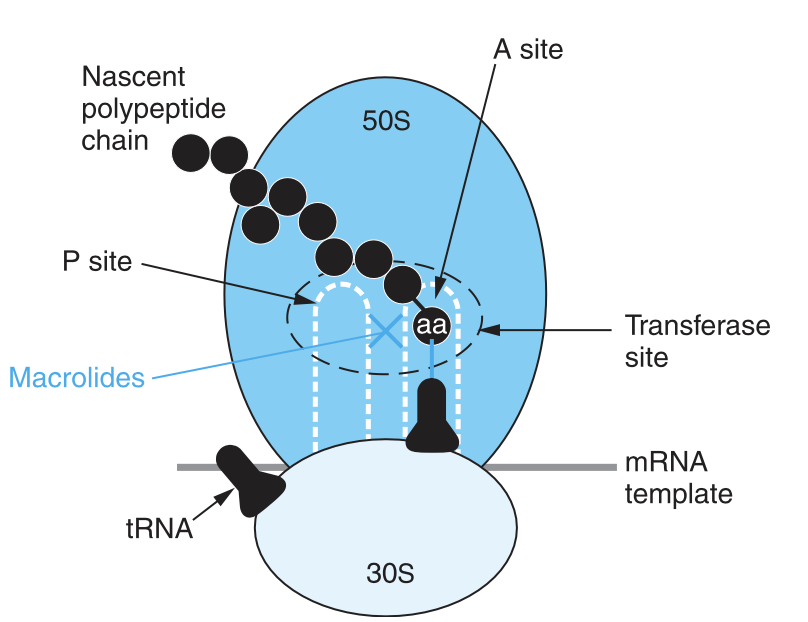
Figure- Inhibition of bacterial protein synthesis by macrolide antibiotics like clarithromycin (Source- Goodman and Gillman book)
- Clarithromycin and its metabolite 14-OH clarithromycin, both acts as a protein synthesis inhibitor. They penetrate bacterial cell wall, reversibly binds to domain V of 23S ribosomal RNA of 50S ribosomal subunit of bacteria and inhibits protein synthesis by inhibiting translocation step. It also affects other steps like transpeptidation.
- Depending on its concentration, it acts either as bacteriostatic or bactericidal.
Pharmacokinetics of clarithromycin
- It is administered orally and undergoes rapid and almost complete absorption from gut. Its absorption is not affected by food. It undergoes first pass metabolism and has short half-life of 3-7 hours. It reaches its peak concentration
- Around 70% of administered drug binds to plasma proteins. It gets widely distributed in tissues. Compared to erythromycin, it has better tissue penetrability. CYP3A4 plays important role in its metabolism. One of its metabolites is 14-hydroxy-clarithromycin which is active.
- Most of the excretion takes via renal route and remaining via feces. Dosage adjustment is required in patients with renal impairment.
Adverse effects
- Common side effects include nausea, vomiting, allergic reaction (fever, eosinophilia, urticaria, dermatitis, lymphadenopathy), diarrhea and epigastric pain. Gastric upset may lead to poor patient compliance.
- Higher dosage may lead to sensorineural hearing loss. This hearing loss is reversible once the drug is stopped. However, in some cases, irreversible sensorineural hearing loss is also observed. It can cause cardiac arrhythmia including QT prolongation with polymorphic ventricular tachycardia, pseudomembranous colitis, and discoloration of teeth.
- There occur chances of superinfection with gram negative bacteria and Candida species.
Drug Interactions
- Clarithromycin can interfere with metabolism of drugs like statins, theophylline, and anti-epileptic agents leading to toxic accumulation of these drugs.
- It may increase risk of QT prolongation when used with other drugs that cause QT prolongation. Such drugs may include amiodarone, procainamide, pimozide, quinidine, sotalol etc.
Contraindications
- It should be used with caution in patients with proarrhythmic condition. When used in combination with proarrhythmic agents, it should be used with caution. It is suggested to use alternative antibiotics, if possible, in heart patients.
- Contraindicated in patients allergic to clarithromycin or other macrolide antibiotics.
- Should not be used if patients have cholestatic jaundice or active liver disease.
- It should be used in pregnancy, only if its benefits outweigh its risks.
Comparison with erythromycin
- Its pharmacokinetic profile is superior compared to erythromycin, which provide benefits of twice daily administration and potential of increased compliance in patients.
- Erythromycin is acid labile whereas clarithromycin is acid stable.
- Erythromycin’s absorption is impaired by food, clarithromycin’s absorption is not impaired by food.
- Clarithromycin shows few GI side effects compared to erythromycin.
References
- Peters DH etal. Clarithromycin A Review of its Antimicrobial Activity, Pharmacokinetic Properties and Therapeutic Potential. Drugs. 1992; 44: 117-164.
- https://go.drugbank.com/drugs/DB01211
- https://pubmed.ncbi.nlm.nih.gov/1421677/
- https://www.ncbi.nlm.nih.gov/books/NBK551495/
- Pharmacology and Pharmacotherapeutics book. 24th edition.
- Goodman and Gillman’s Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology. 6th edition.