- Calcium channel blocker (CCBs) also known as calcium channel antagonist or calcium antagonist are group of medicines that block movement of calcium through calcium channel.
- They are used to treat various conditions associated with heart.
Classification of calcium channel blockers
They are divided into 3 chemical classes having different pharmacokinetic parameter and clinical uses.
Diphenylalkylamine: e.g. Verapamil
Benzothiazepines: e.g. Diltiazem
Dihydropyridine: e.g. Amlodipine, Nifedipine, Felodipine, Nicardipine, Isradipine and Nislodipine.
Mechanism of action of calcium channel blockers
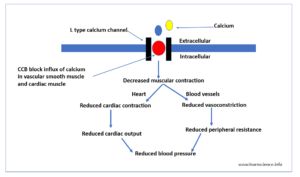
Figure- Mechanism of action of Calcium Channel Blockers (CCBs)
- Calcium play important role in excitation-contraction coupling in the skeletal, cardiac and smooth muscle. The contractility of cardiac and vascular smooth muscle is highly dependent on extracellular calcium. There are two types of calcium channel in heart: L channel and T channel.
- CCB bind to alpha-1 subunit of L channel and inhibit entry of calcium into cardiac and vascular smooth muscle. This causes decrease in intracellular calcium leading to relaxation of vascular smooth muscle, vasodilation and ultimately reduce blood pressure. It reduces contraction in cardiac muscle and slows sinus pacemaker and AV conduction.
- Dihydropyridine CCBs are more potent vasodilators than non-dihydropyridine (diphenylalkylamine and benzothiazepines) agents, whereas the latter have more marked negative inotropic effects. Both subclasses have a similar capacity to lower BP; however, non-dihydropyridine are found to be more advantageous in the management of patients with chronic kidney disease and diabetic nephropathy.
Pharmacological Actions of calcium channel blockers
Cardiovascular Actions
- They relax vascular smooth muscle and decrease vascular resistance and BP.
- They possess negative ionotropic effect: i.e. they decrease myocardial contractility, cardiac workload and oxygen consumption. This effect is responsible for its anti-anginal effect.
- They improve coronary blood flow and dilates large epicardial branches of coronary arteries as well as smaller intramyocardial coronary arterioles. CCBs prevent spasm in diseases, atherosclerotic coronary arteries.
- They also possess antiarrhythmic effect by decreasing rate of discharge of SA node, slowing the AV conduction, suppressing ectopic pacemaker activity and increasing refractoriness of the AV node.
Non-cardiovascular actions
- In kidney, they increase renal blood flow, dilate afferent arterioles, increase glomerular filtration rate and produce natriuresis.
Pharmacokinetics
- Their absorption is nearly complete after oral administration. However, in some cases bioavailability may be reduced due to first pass metabolism.
- They start acting within 30-60 minutes of an oral dose. Most of them have short half-lives (3-8 hours) except some longer acting agents like amlodipine, isradipine and felodipine. Those having short half- lives are available in sustained release formulation to permit once daily dosing.
- They bind extensively to plasma proteins.
- Metabolites of some CCB are active whereas of some are less active or inactive. For example, norverapamil, metabolite of verapamil is active but less potent than parent compound. Metabolite of diltiazem- desacetyldiltiazem is half-potent as parent compound.
- In cirrhosis patients, their bioavailability and half-life may increase so dosage should be adjusted accordingly. Their half-life may be longer in elder patients.
Therapeutic Uses
- Used as initial therapy or add on therapy for treating hypertension. They are used alone or in combination with other anti-hypertensives. They are useful in hypertensive patients with asthma, diabetes or peripheral vascular disease (they don’t deteriorate these conditions unlike beta-blockers).
- Useful in treatment of angina pectoris.
- Verapamil and diltiazem are used to lower heart rate during arrhythmia, especially atrial fibrillation and atrial flutter.
- For prevention of migraine attacks.
- Nifedipine can be used orally/sublingually as tocolytics. It is safe, can be administered at any gestational age and helps in reducing neonatal complications.
- Nifedipine is effective in Raynaud’s syndrome.
- May be beneficial in exercise induced asthma.
Adverse Effects
- They are usually well tolerated.
- The most common side effects of dihydropyridines are due to excessive vasodilation. They cause hypotension, headache, dizziness, flushing and nausea.
- Some other side effects are constipation, coughing, wheezing, gingival hyperplasia, peripheral and pulmonary edema. Constipation is more common with verapamil.
- Negative ionotropic effect of verapamil may exacerbate cardiac failure.
Drug Interaction
- IV verapamil when used together with betablocker can cause circulatory collapse.
- Verapamil and diltiazem increase plasma level of digoxin and cyclosporine.
- Drugs like rifampin decreases plasma level of verapamil and diltiazem whereas their plasma level is increased by drugs like erythromycin and cimetidine.
- CCBs when administered together with products containing grapefruit juice, can affect heart rate and blood pressure. It can cause headache and dizziness. So, grapefruit juice should be avoided while taking CCBs.
Contraindication
- Contraindicated in patients who are allergic to components of given preparation.
- Verapamil and diltiazem are contraindicated in hypotension, sick sinus syndrome, second- or third-degree AV block and accessory bypass tract.
- Verapamil is contraindicated in patients with severe left ventricular dysfunction and diltiazem is contraindicated in acute myocardial infarction and pulmonary congestion x-ray.
- Contraindicated in myocardial depression, bradycardia, heart block and clinical heart failure.
Reference
- https://www.healio.com/cardiology/learn-the-heart/cardiology-review/topic-reviews/calcium-channel-blockers
- Chiu KY, Li JG, Lin Y. Calcium channel blockers for lung function improvement in asthma: A systematic review and meta-analysis. Annals of Allergy, Asthma & Immunology. 2017; 119(6): 518-523.e3.
- Frishman WH. Calcium Channel Blockers: Differences Between Subclasses. American Journal of Cardiovascular Drugs. 2007; 7: 17–23.
- Albrecht FE, Asico LD, Jose PA, Eisner GM. Mechanism of calcium channel blocker (CCB)-mediated natriuresis. Pediatric Research. 1996; 39: 357.
- Sica DA. Pharmacotherapy Review: Calcium Channel Blockers. The journal of clinical hypertension. 2006; 8(1);53-56.
- Elliott WJ, Ram VS. Calcium Channel Blockers. The Journal of Clinical Hypertension. 2011; 13(9): 687-689.
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- A Textbook of Clinical Pharmacology and Therapeutics. 5th edition.