What are Thyroid hormones?
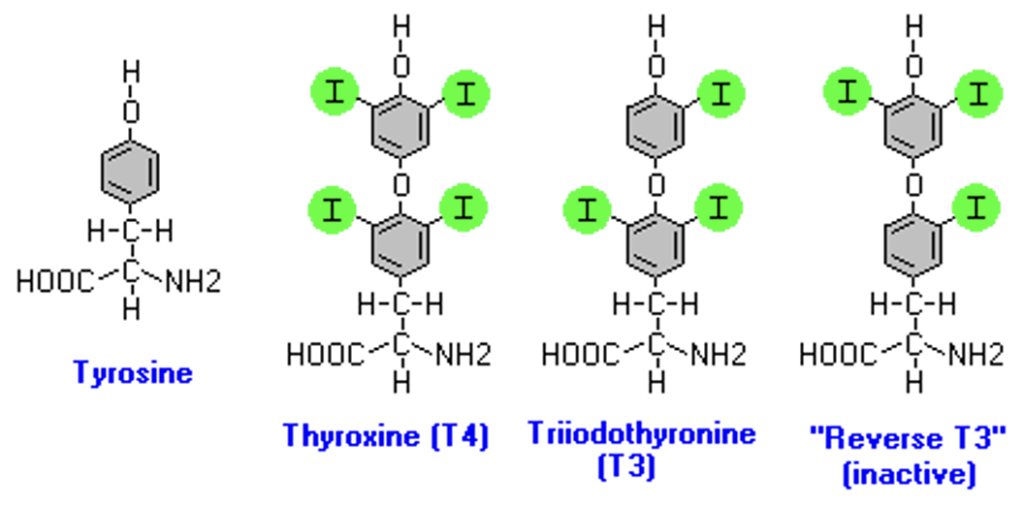
- Thyroid hormones are two hormones produced and released by thyroid gland namely triiodothyronine (T3) and thyroxine (T4). T3 and T4 are partially composed of iodine. They are tyrosine-based hormones which are primarily responsible for regulation of metabolism.
- Inadequate secretion of thyroid hormone (hypothyroidism) results in bradycardia, poor resistance to cold, and mental and physical slowing. In children, this can cause mental retardation and dwarfism. Excess secretion of thyroid hormone (hyperthyroidism) can cause tachycardia and cardiac arrhythmias, body wasting, nervousness, tremor, and heat intolerance
Functions of thyroid hormones
- Thyroid hormones promote growth and protein synthesis.
- Essential for intra-uterine tissue differentiation and extra-uterine growth.
- They help in regulation of BMR (Basal Metabolic Rate) by stimulating oxygen consumption and heat production in all tissues except the brain, gonads, lymph nodes, spleen, thymus and dermis.
- They help in normal maturation and function of central nervous system.
- Thyroxine stimulate rate and force of contraction of myocardium and increase cardiac output.
- They help in regulating protein, fat and carbohydrate metabolism.
Synthesis of thyroid hormones
- The synthesis of thyroid hormones occurs in thyroid gland; a butterfly shaped endocrine gland located in the neck. Normal thyroid hormone synthesis requires a normally developed thyroid gland, an adequate nutritional iodide intake and a series of highly regulated biochemical steps.
- It comprises of following steps:
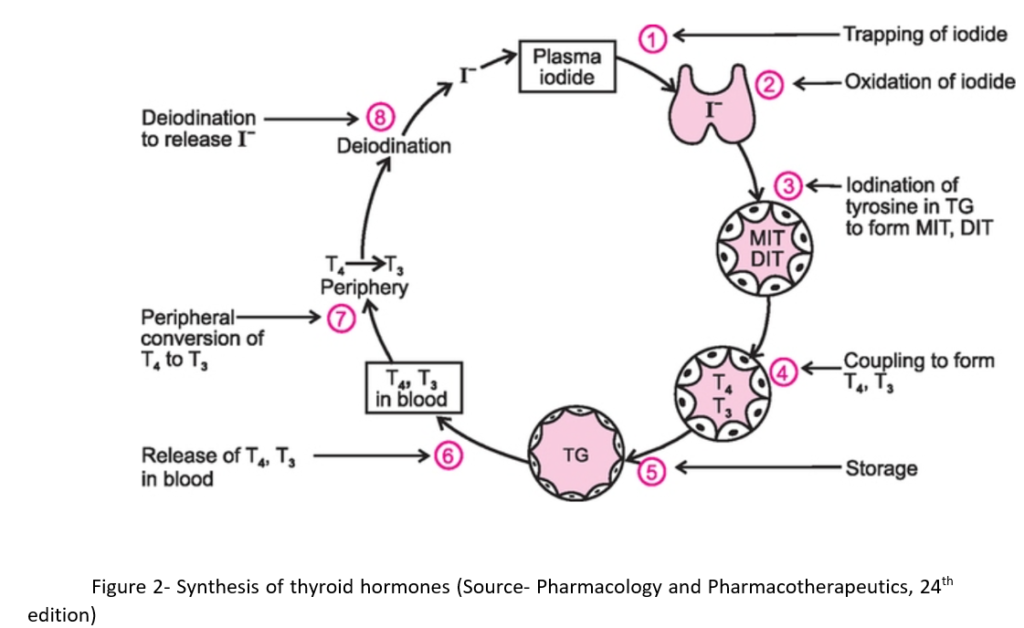
Iodide trapping
- Iodine is important for thyroid health as it is the building block of thyroid hormones. As our body doesn’t produce iodine, we should take iodine in the form of our food. The iodide which we intake through our food is carried from upper GI tract in plasma as inorganic iodide.
- Thyroid gland traps the plasma iodide circulating through it via a specific, membrane-bound protein termed as sodium-iodide symporter (NIS). NIS is stimulated by thyroid stimulating hormone (TSH) which is controlled by an autoregulatory mechanism.
- The NIS is inhibited by ions like thiocyanate and perchlorate. Thyroid gland should compete with kidney (which excrete iodine in urine) and in less extent with mammary gland, liver, salivary gland, intestinal mucosa and placenta to trap plasma iodide.
Organic binding of iodine
- Thyroid follicles consist of a central cavity called colloid filled with sticky fluid which is bordered by wall of epithelial follicle cells.
- The iodide is moved to follicular cells surrounding colloid and oxidized by hydrogen peroxidase (H2O2) and thyroid peroxidase to hypo iodate. Hypo iodate iodinates tyrosyl residues in thyroglobulin (TG) to form mono- and diiodotyrosine (MIT and DIT) successively. Both reactions are stimulated by TSH.
- Thyroid peroxidase is a heme containing enzyme that utilizes hydrogen peroxide as oxidant. The peroxidase is membrane bound. Hydrogen peroxide is formed near its site of utilization.
Coupling
- Two diiodotyrosine (DIT) couple together to from thyroxine (T4) and one monoiodotyrosine (MIT) and one diiodotyrosine (DIT) couple together to form triiodothyronine (T3). The reaction is catalyzed by same peroxidases involved in 2nd step.
- This reaction occurs when MIT and DIT are bound within thyroglobulin molecule by peptide bond.
Hormonal Release
- T3 and T4 are synthesized and stored in thyroglobulin. The proteolysis of TG takes place with the help of protease in presence of TSH. It is initiated by endocytosis of colloid from follicular lumen. TSH enhances TG degradation by stimulating activity of several lysosomal thiol endopeptidases.
- Finally, hormones are released and exit the cell and passes to the blood stream to be delivered to various parts of body.
Peripheral conversion of T4 to T3
- The normal daily production of T4 is 70–90 µg, while that of T3 is 15–30 µg.
- The T3 and T4 hormones in blood stream are bound to special transport proteins called thyroxine-binding globulins (TBGs). This binding doesn’t allow diffusion of T3 and T4 into body cells. However, when blood levels of thyroid hormones start to decline, T3 and T4 are released into their target cells.
- As T3 is more potent than T4, many cells convert T4 to T3 by removing an iodine atom. About 40 % of T4 released by thyroid gland is converted into T3 by peripheral tissues and thyroid.
References
- https://www.drmarkneumann.com/blog/2019/10/22/5-steps-in-thyroid-hormone-synthesis
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- Clinical Management of Thyroid Disease.