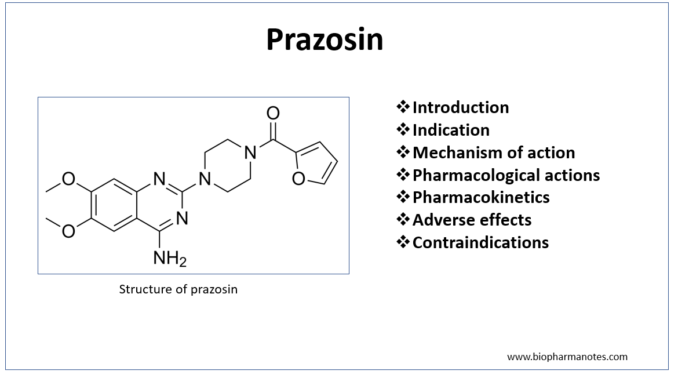
- Prazosin is selective α-1 blocker which is used to treat hypertension. It got its FDA approval for it’s medical use in 1988. Chemically, it is a quinazoline derivative and exert peripheral vasodilation effect.
Indications of prazosin
- To treat hypertension. It is not used as first line drug for hypertension. Prazosin is used alone or in combination with other agents. It is mostly used to treat moderate to severe hypertension as adjunct with beta- blockers and diuretics.
- To treat CHF (Congestive Heart failure).
- In benign prostatic hyperplasia and prostatism with obstructive symptoms.
- Some off- label uses are post-traumatic stress disorder (PTSD), Raynaud phenomenon, pheochromocytoma and scorpion envenomation.
Mechanism of action of prazosin
- It is an alpha-1 adrenergic receptor antagonist. Alpha adrenergic receptors play important role in regulation of blood pressure. α-1 receptors are present in smooth muscles like wall of blood vessels (arteries and veins), urethra, brain and iris dilator muscle. Prazosin competitively blocks α-1 receptors and cause both arterial and venous smooth muscle relaxation leading to decrease in blood pressure.
- It can cross BBB (blood brain barrier) and hence has some cognitive effects and use in PTSD.
Pharmacological action of prazosin
- It is effective in controlling both supine and standing BP with minimum chances of postural hypotension. It decreases cardiac preload which can cause little increase in cardiac output and rate. Chances of tachycardia is minimum as prazosin doesn’t have effect on presynaptic α-2 receptors.
- Prazosin may decrease total and LDL cholesterol and cause increase in HDL cholesterol. And also causes decrease in central sympathetic tone. It doesn’t have major affect on renal function, cardiac output and RAAS (Renin Angiotensin Aldosterone System).
- It doesn’t disturb carbohydrate metabolism; hence it is suitable for diabetic patients. However, it is not used if patients have neuropathy.
Pharmacokinetics
- It is administered through oral administration and is well absorbed from gut. Bioavailability after oral administration is 50-70%.
- It is highly bound to proteins. The binding proteins are albumin and alpha 1- acid glycoprotein.
- Metabolism takes place in liver. It has plasma half-life of 2-3 hours and peak plasma concentration reaches is observed within 1-3 hours after oral dose. The half-life may increase up to 6-8 hours in case of CHF.
Adverse effects
- The common side effect is postural hypotension which occur after initial dose or after rapid increase in dose. One can minimize it by starting with lowest dose possible, administering first dose at night before bedtime and by increasing dose gradually. Some patients may get first dose effect following the first dose which is characterized by palpitation, postural hypotension and collapse.
- Some other common side effects are headache, dizziness, drowsiness, nausea, palpitation and lack of energy.
- In patient with cataract surgeries, administration of prazosin may cause intraoperative floppy iris syndrome (IFIS) due to blockade of α-2 receptors on iris dilator muscle.
Contraindication
- Patients who are allergic to prazosin or have history of previous anaphylaxis to prazosin.
- It is category C drug in pregnancy, which means that there is insufficient data to support its use in pregnancy.
- It should be used with caution in patient with cataract and in patient with hypotension.
References
- https://www.statpearls.com/ArticleLibrary/viewarticle/929
- https://go.drugbank.com/drugs/DB00457
- Pharmacology and Pharmacotherapeutics book. 24th edition.
- Goodman and Gillman’s Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology. 6th edition.
- Essentials of Medical Pharmacology. 7th edition.
- Brogden et al. Prazosin: A Review of its Pharmacological Properties and Therapeutic Efficacy in Hypertension. Drugs volume 1977; 14: 163–197.