
What is schizophrenia?
- Schizophrenia is a complex, chronic mental health disorder that alters an individual’s perception, thought, affect and behavior. The word ‘schizophrenia’ was derived from a Greek word meaning ‘split mind’. The harmonious working of the mind is split.
- The symptoms are divided into three categories; positive, negative and cognitive. Positive symptoms include hallucination (e.g. hearing god talking), delusion (false beliefs), illusion (e.g. mistaking a rope for snake), thought disorder which may occur as distorted speech. Negative symptoms include social withdrawal, loss of motivation and emotional blunting. Cognitive symptoms include cognitive dysfunctions.
- Its etiology is not exactly known. It is believed to be due to abnormal activity at dopamine receptor sites.
- According to one study, the incidence rate of schizophrenia was noted to be 15.2 per 100,000. The incidence rate was higher in males, urban and migrant population. Genetic factor also plays important role in the cause of schizophrenia. Environmental and social factor may play role in development of schizophrenia in those who are vulnerable to the disorder.
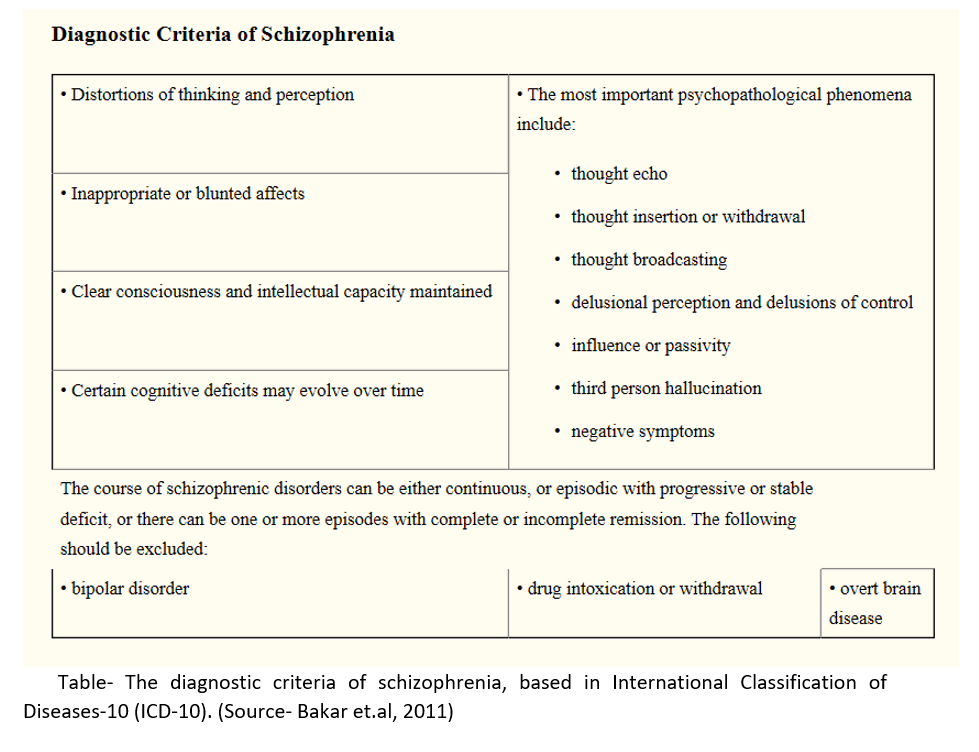
Diagnosis of schizophrenia
- People who develop schizophrenia should be diagnosed and treated early.
Management of schizophrenia
- Management of schizophrenia should be complete package which includes individually- tailored medication, an appropriate psychosocial and service level interventions.
- The goal of treatment is to alleviate symptoms, prevent relapse and increase adaptive functioning to integrate patient back into community.
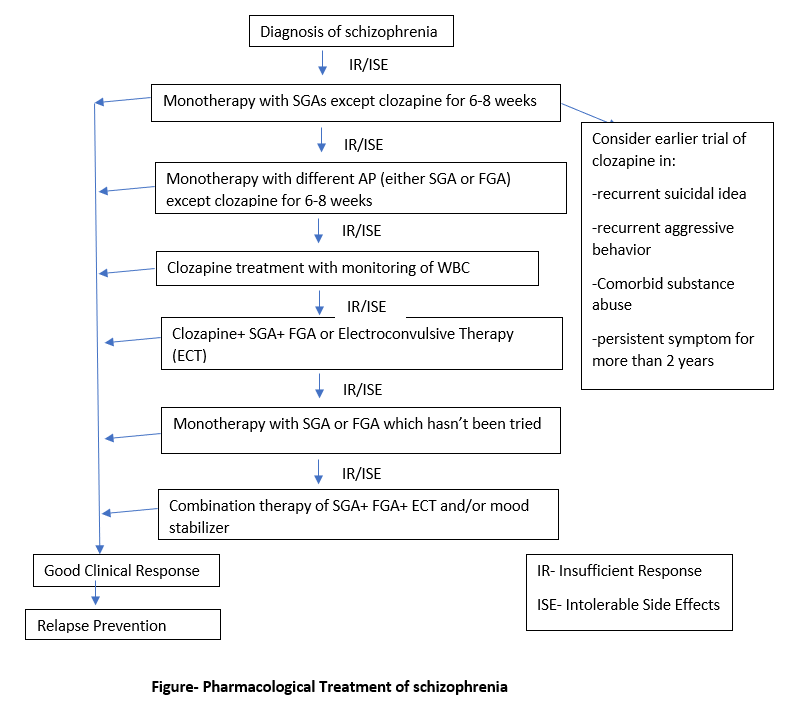
Pharmacological Treatment
- In the event of an acute psychotic episode, drug therapy should be administered immediately. Prompt initiation of drug treatment should be started, specially within five years after the first acute episode. During the first seven days of treatment, the goal is to decrease hostility and to return the patient to normal functioning.
- Antipsychotics (AP) used don’t cure schizophrenia but alleviate symptoms and make patient more acceptable and cooperative. In 70 % of the cases, patient show favorable response.
- Antipsychotics can be classified into two types; first generation (FGA- e.g. chlorpromazine, haloperidol, trifluperidol, molindone etc ) and second-generation antipsychotics (SGA- e.g. olanzapine, sulpiride, risperidone, quetiapine, clozapine).
- SGAs (except clozapine) are preferred for 1st line treatment because of their fewer extrapyramidal symptoms.. Clozapine is not recommended because of its risk of agranulocytosis.
- The drugs are started in the smallest possible dose and increased gradually according to need.
Things to consider during pharmacological treatment of schizophrenia
- Before starting new antipsychotic agents, the complete review of patient’s medication history should be done. The routine use of two or more antipsychotics together is not recommended due to risk of drug interactions, non-adherence and medication errors.
- Some patients may not be adherent to oral medication. If it is due to adverse effects of treatment, an oral medication with more favorable side-effects profile should be considered. If it is due to patient’s negligence, long acting injectable (LAI) antipsychotic agents may be administered. Before starting LAI therapy, a short trial using oral form of LAI should be performed to check tolerability.
- As chances of relapse persist, the drug should be continued in smaller maintenance dose for a long time (lifelong in some cases) even after first episode of illness. The withdrawal of drugs should be done slowly (over 6-12 months). In a patient with history of relapse, longer maintenance period is recommended.
- Both FGAs and SGAs are associated with several adverse effects. Weight gain, extrapyramidal symptoms, leukopenia, seizures are some common adverse effects observed. Proper care and attention are needed to minimize such effects.
Non-Pharmacological Treatment
- Pharmacotherapy is main stay in management of schizophrenia, but residual symptoms may persist. So, non-pharmacological treatment like psychotherapy should be considered. It helps to fill the gap of pharmacological therapy and ensure adherence of patients to their medications.
- Psychotherapeutic approaches include counselling, personal therapy, educating patients about their illness and risks and effectiveness of treatment, social skills therapy and vocational sheltered employment rehabilitation therapy, cognitive behavioral therapy (CBT).
- Psychosocial interventions help in improving individual’s ability to handle stressful life events, increase adherence to medication, promote better communication and coping skills, improve quality of life and promote recovery and reintegration.
- The treatment should also focus on educating family members on how to monitor the patient and when to report adverse effects to doctor. Treatment programs that encourage family support have been found to improve social attributes of patient and decrease relapse.
References
- Kahn RS, Sommer IE, Murray RM, Weinberger DR, Cannon TD, Kane JM et al. Schizophrenia. Nature Reviews Disease Primers. 2015; 1:1-23.
- Picchioni MM, Murray RM. Schizophrenia. BMJ. 2007 Jul 14; 335(7610): 91–95.
- Patel KR, Cherian J, Gohil K, Atkinson D. Schizophrenia: Overview and Treatment Options. P T. 2014 Sep; 39(9): 638–645.
- Bakar AKA, Jali N, Yusof MAM. Management of Schizophrenia in Adults. Malays Fam Physician. 2011; 6(2-3): 91–93.
- Pharmacology and Pharmacotherapeutics 24th edition. Page no- 205-218.