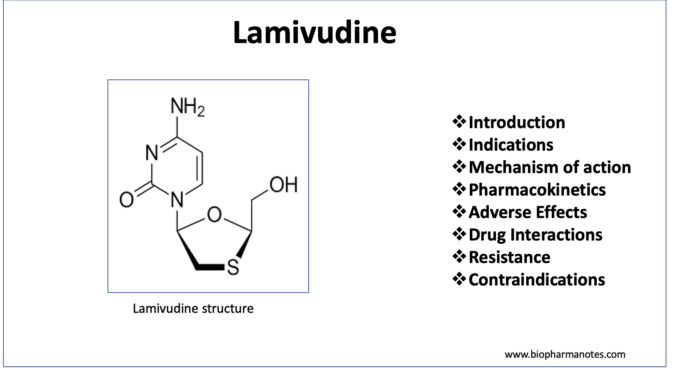
- Lamivudine is nucleoside reverse transcriptase inhibitor (NRTIs) and is active against HIV1 (Human Immunodeficiency Virus 1), HIV2 (Human Immunodeficiency Virus 2) and HBV (Hepatitis B Virus). It is a synthetic nucleoside analogue.
- Lamivudine is also commonly known as 3TC (2’,3’-dideoxy-3’-thiacytidine). It was approved by FDA for HIV treatment in 1995 in combination therapy with zidovudine and approved for HBV treatment in 1998. It is also included in World Health Organization’s List of Essential Medicines.
Indications of Lamivudine
- Used in combination with other antiretroviral agents to treat HIV-1 infection. It helps to reduce viral load, increase CD4+ cells count, alleviate disease symptoms and improve quality of life of patients and also prolong patient’s life.
- Used as monotherapy in treatment of Hepatitis B Virus infection.
Mechanism of action of Lamivudine
- It is a reverse transcriptase inhibitor and is analogue of cytidine. Inside cells, it is phosphorylated to triphosphate form, lamivudine triphosphate (L-TP or 3TC-TP).
- This triphosphate form is active and competes with natural substrate- cytidine triphosphate and is incorporated into viral DNA by reverse transcriptase of both HIV-1 and HBV. As, it doesn’t have 3’- hydroxyl group, a 3’,5’- phosphodiester bond cannot be formed between incoming nucleoside triphosphate and hence, growing DNA chain cannot be formed. This results in termination of viral DNA chain elongation.
- The active form of lamivudine has low affinity for human DNA polymerases.
Pharmacokinetics of Lamivudine
- It is absorbed rapidly after oral administration and its oral bioavailability is more than 80%. Its bioavailability is not affected by food so it can be taken with or without food. Lamivudine is available as oral tablet or liquid formulation.
- It is distributed in total body fluid and extravascular spaces. It has long intracellular half-life (around 15.5 hours in HIV infected cells and around 19 hours in HBV infected cells). Its mean elimination half-life is around 5-7 hours. It can cross placenta and is also found in breast milk.
- Majority portion of drug is excreted unchanged via urine. Small amount is also excreted as its only known metabolite, trans sulfoxide metabolite. Dosage adjustment is required in patients with low creatinine clearance (<50 mL/min).
Adverse effects
- It has good safety profile and is one of the least toxic antiretroviral agents.
- It can cause side effects like headache, GI disturbances (nausea, vomiting, abdominal pain, diarrhea), fever and weight loss. Some of its rare but severe effects include muscle pain, muscle weakness, aplastic anemia, pancreatitis (specially in children), lactic acidosis with hepatic steatosis and Steven Johnson syndrome.
Drug Interactions
- As it is not metabolized by CYP450 pathway, it doesn’t have numerous drug interactions. Some few drug interactions include increase in plasma concentration of lamivudine by drugs like zidovudine, ribavirin, indinavir, trimethoprim and interferon alpha blockers.
- Concurrent administration of sorbitol may decrease plasma concentration of lamivudine.
Resistance
- Development of resistance to lamivudine is recognized problem. Resistance to lamivudine may be developed due to various reasons. One of the reasons is mutation in single amino acid at codon 184. This mutation can decrease sensitivity of lamivudine in drastic way (around 1000 folds). This mutation however doesn’t affect zidovudine.
- Other common mutations which cause resistance occur in highly conserved YMDD motif in C domain of viral polymerase and are also associated with compensatory mutation in proximal B domain.
Contraindications
- Contraindicated in patients with known hypersensitivity to lamivudine or other components of the formulation.
References
- https://www.ncbi.nlm.nih.gov/books/NBK559252/
- https://go.drugbank.com/drugs/DB00709
- https://pubchem.ncbi.nlm.nih.gov/compound/Lamivudine
- Quercia R et al. Twenty-Five Years of Lamivudine: Current and Future Use for the Treatment of HIV-1 Infection. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2018; 78(2):1.
- Fischer KP et al. Lamivudine resistance in hepatitis B: mechanisms and clinical implications. Drug Resist Updat. 2001 Apr; 4(2): 118-28.
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- A textbook of Clinical Pharmacology and Therapeutics. 5th edition.