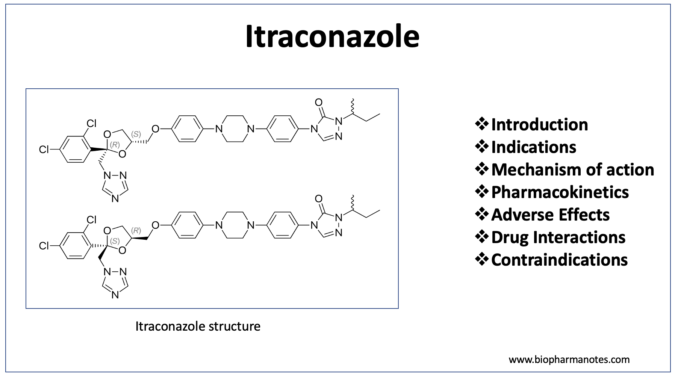
- Itraconazole is broad spectrum antifungal agent. It is a synthetic triazole and has activity like ketoconazole. Other triazole antifungals available in medical field includes fluconazole, voriconazole and Posaconazole.
- It is included in World Health Organization’s List of Essential Medicines.
Indications of itraconazole
- It is used in treating fungal infections like sporotrichosis, blastomycosis, histoplasmosis and Paracoccidioidomycosis.
- IV itraconazole is used in prophylaxis of febrile neutropenic patients who are not responding to antibiotics and are at high risk of developing fungal infections. It is also used as prophylactic treatment in other patients who are at risk of developing fungal infections including HIV patients, patients who are on chemotherapy or patients who have received organ transplant.
- It is not preferred agent for treatment of infections caused by Candida and Aspergillus species as new and effective agents are available for these infections.
- Some of its off- label uses are moderate to severe seborrheic dermatitis, other topical mycoses
Mechanism of action of itraconazole
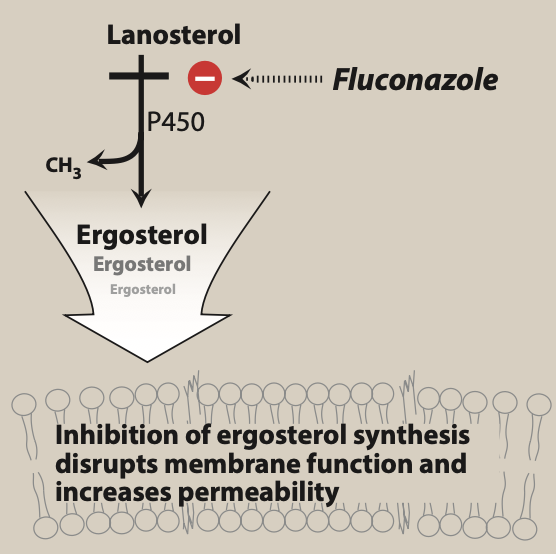
Figure- Mechanism of action of azole antifungal agents including itraconazole (source- Lippincott’s Illustrated Reviews Pharmacology, 6th edition)
- Itraconazole acts by inhibiting ergosterol synthesis. Ergosterol is major component of cell membrane of fungi.
- It binds to and inhibits fungal cytochrome P450 enzyme, C-14 a-demethylase which is involved in 14- alpha demethylation reaction of lanosterol to ergosterol. This inhibition in ergosterol synthesis cause impairment in membrane structure and function and results in inhibition of fungal cell growth.
Pharmacokinetics of itraconazole
- It is administered via oral or IV route. It is weak base and gets ionized at lower pH. Hence, acidic environment is required for dissolution and absorption. The oral capsule is generally taken with food or acidic beverage to increase absorption. However, in case of itraconazole solution, the food decreases its absorption, so it is taken on empty stomach. Absorption is variable.
- It is metabolized extensively in liver by CYP3A4 enzymes. Its major metabolite is hydroxy- itraconazole which also possess antifungal activity. It is lipophilic nd extensively binds to plasma proteins (around 99%). It gets distributed in most of the body tissues including skin, nails, bone and adipose tissues.
- Its half-life is around 30 hours. It takes more than 4 days to reach steady state level. Hence, loading doses are used when using itraconazole for treating deep mycoses.
Adverse effects
- Common side effects include nausea, vomiting and rashes. Other side effects include hypokalemia, hypertriglyceridemia and elevated serum aminotransferase level. Rashes may be the reason for discontinuation of drug in many patients. Other side effects can be managed by dosage reduction.
- It can also cause GI side effects like abdominal cramps, diarrhea, and nausea. Chances of GI side effects are more with oral solution compared to capsule.
- It can cause congestive heart failure in patients with impaired ventricular function. Chances of hepatotoxicity is rare.
Drug Interactions
- As it is metabolized by CYP3A4 enzymes, it has potential for many drug- drug interactions. Concurrent administration of itraconazole with oral antidiabetic drugs may lead to enhancement in effects of antidiabetic drugs leading to severe hypoglycemia.
- It can enhance sedative effects of drugs like midazolam and triazolam. Coadministration of itraconazole and drugs like cisapride, astemizole may increase risk of serious disturbance in cardiac rhythm.
Contraindications
- Contraindicated in patients with known hypersensitivity to itraconazole.
- It is avoided in pregnancy until the potential benefits outweigh the risk of adverse effects to fetus.
- Due to its negative ionotropic effect, it is avoided in patients with ventricular dysfunction such as heart failure.
- IV formulation of itraconazole is contraindicated in patients with creatinine clearance less than 30 mL/min.
- Contraindicated in patients with impaired hepatic function.
References
- https://www.statpearls.com/ArticleLibrary/viewarticle/23794
- Beule KD e t al. Pharmacology of Itraconazole. Drugs. 2001; 61: 27–37.
- Doncker PD et al. Itraconazole: What clinicians should know? Indian Journal of Drugs in Dermatology. 2017; 3(1): 4-10.
- https://en.wikipedia.org/wiki/Itraconazole
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.