Anatomy of Cornea
- Cornea is the transparent, outermost, dome-shaped layer of the eye that is in front of the iris and pupil of the eye. Light rays from outside world first pass through the cornea before reaching the lens. While using the contact lens, the contact lens rests on the cornea.
- Cornea is connected smoothly to the white sclera.
- It is about 12 mm in diameter. In most people, it is somewhat oval and is thicker at edges than at the center. The cornea doesn’t contain blood vessels, except at its margin. It contains many nerves and is very sensitive to pain and touch. The curvature of the cornea is spherical in infants and changes with age which give it’s focusing power.
- As it doesn’t contain nutrient supplying blood vessels, it is nourished and provided with oxygen anteriorly by tears and bathed posteriorly by aqueous humor present in aqueous chamber.
- Cornea is composed of five layers;
- Epithelium
- Bowman’s layer
- Stroma
- Descemet’s membrane
- Endothelium
Corneal Epithelium
- This outermost layer of cornea is 5-7 cells thick and measures about 50 microns. It is responsible for less than ten % thickness of cornea.
- It is an important barrier to infection. Corneal infection or scratch can cause intense pain, tearing, light sensitivity and sensation of something being on the eye. However, corneal epithelium can heal quickly in most situations as epithelial cells are constantly produced and sloughed off in the tear layer.
- It absorbs nutrients and oxygen from the tears and supply it to other parts of cornea.
Bowman’s layer
- Bowman’s layer is a very thin layer of dense fibrous sheet of connective tissues measuring around 8-14 microns. It is absent or very thin in non-primates. It is also called Bowman’s membrane or the anterior limiting membrane.
- This layer acts as transition between the corneal epithelium and stroma. It prevents direct traumatic contact of the corneal stroma and is involved in stromal wound healing.
Corneal stroma
- Corneal stroma constitutes around 90 % thickness of whole cornea and is about 500 microns thick. It is the thickets layer of the cornea.
- It is composed of the collagen fibers which are uniform in size and are arranged in uniform, geometrical pattern. These collagen fibrils are superimposed on one another to form 200-300 flat bundles called lamellae. The fibrils of each lamella are parallel with each other. This regular arrangement is responsible for cornea’s transparency.
- During infection or trauma of cornea, the collagen laid down in the repair process is not regularly arranged resulting in opaque patch or scar.
Descemet’s membrane
- It is a very thin layer of cells between corneal stroma and corneal endothelium. It is also known as posterior limiting membrane.
- Its thickness may vary according to age. In children, it may be around 5 microns thick whereas in adults, the thickness may be around 15 microns.
Corneal endothelium
- It is the innermost layer of the cornea consisting of single layer of cells. It measures around 5 microns thick. Most of the endothelial cells have 6 sides (hexagonal), but some may be pentagonal or heptagonal too.
- The back of endothelium is bathed in the clear aqueous humor. It helps in regulating fluid and solute transport between aqueous and stromal compartments.
- Unlike the corneal epithelium, these cells don’t regenerate. When endothelial cells are lost, existing cells stretch to occupy the space left behind. This prevents swelling of cornea due to excessive fluids. However, if critical number of endothelial cells are lost, cornea can swell causing pain and decreased vision.
Function of cornea
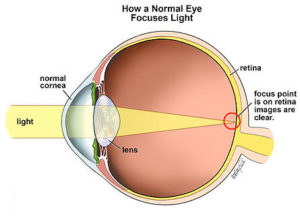
Figure 1- Light rays passes through cornea and lens and is focused on retina.
- It is like a window that control and focuses the entry of light into the eye.
- Cornea refracts light before it passes to the iris and lens. The lens further refracts the light to refine the image projected into retina. It provides 65-75 % of focusing power of an eye.
- Cornea acts as filter and screen out some most harmful UV wavelengths in sunlight. It also protects eyes from germs or dust by working together with eyelids, eye sockets, tears and the sclera.
- Its smoothness, shape and as well as transparency are important for proper functioning of eye.
Cornea Problems
- Cornea can be affected by number of diseases. Corneal disease is one of the leading causes of blindness in the world. Cornea is also subjected to risk of abrasions like scratching. Minor abrasions affecting only epithelium may heal itself. Whereas, deeper abrasions can impair vision and cause blindness.
- Let’s learn about some common corneal problems.
-
Corneal ulcer
- It is an erosion or open sore on the surface of cornea. As it can permanently affect sight, it is considered as ophthalmic emergencies.
- Infectious corneal ulcer is a major cause of corneal blindness. About 2 million new corneal ulcers occur every year only in Asia and Africa.
- It may be caused due to germs (bacteria, virus, fungi), injury or severe allergic disease. Wearing contact lens may be the major risk factor for corneal ulcer.
2. Arcus senilis

Figure 2- Appearance or corneal arcus or arcus senilis
- It is also known as corneal arcus or corneal senilis. It is lipid deposits that forms ring shape at corneoscleral limbus. They are usually grey or white and are opaque. They can grow with time can cover the entire cornea.
- Its prevalence increases with advancing age. It may be associated with hypercholesterolemia, blood pressure, smoking, alcohol, age, diabetes and coronary heart disease.
3. Corneal dystrophy
- They are inherited disorders that affect any layer of cornea and are usually progressive. Some of these dystrophies may not be progressive or inherited.
- There are more than 20 types, each with different symptoms. Some type of corneal dystrophies is Lisch corneal dystrophy, macular corneal dystrophy, Fuchs’s endothelial corneal dystrophy, Reis-Buckler’s corneal dystrophy, posterior polymorphous corneal dystrophy etc.
4. Keratitis

Figure 3- an eye with non-ulcerative sterile keratitis
- It is characterized by inflammation of cornea and may be accompanied by pain, red eye, light sensitivity and impaired eyesight.
- Keratitis may be fungal (fungal keratitis), amoebic (acanthamoeba keratitis), viral (herpes simplex keratitis), parasitic (onchocercal keratitis) or bacterial (bacterial keratitis). Epithelial injury and defects play important role in making eye susceptible to corneal pathogens. Contact lens wearers are at major risk of developing keratitis more often.
5. Keratoconus (degenerative disease of cornea)

Figure 4- An eye with keratoconus
- It is a degenerative disease which causes thinning, bulging and deformation of cornea. It can lead to visual impairment and corneal ectasia if untreated. Its etiology is not clear.
- Treatment begins first with contact lenses and may progress to surgery, cross-linking and corneal transplantation.
5. Corneal ectasia
- It is similar to keratoconus but is of different origin. In this loss of substance or scarring of cornea may cause thin layer of cornea and its bulging. For example, during LASIK eye surgery.
6. Corneal abrasion (Scratched cornea)

Figure 5- Corneal abrasion
- It is one of the most common ophthalmological injuries in which the cornea is scratched due to foreign bodies. A scratched cornea can cause red eyes, light sensitivity and pain or discomfort.
- Dry eyes can increase risk of corneal abrasion.
References
- Munjal A, Kaufman EJ. Arcus Senilis (Corneal Arcus). In: StatPearls. Treasure Island (FL): StatPearls Publishing; February 1, 2020.
- Fernandez A, Sorokin A, Thompson PD. Corneal arcus as coronary artery disease risk factor Atherosclerosis. 2007; 193(2): 235-40.
- AlMahmoud T, Elhanan M, Elshamsy MH, Alshamsi HN, Abu- Zidan FM. Management of infective corneal ulcers in a high-income developing country. Medicine (Baltimore). 2019; 98(51): e18243.
- Soh YQ, Kocaba V, Weiss JS, Jurkunas UV, Kinoshita S, Aldave AJ et al. Corneal dystrophies. Nature Reviews Disease Primers. 2020; 6(46).
- Lakhundi S, Siddiqui R, Khan NA. Pathogenesis of microbial keratitis. Microb Pathog. 2017; 104: 97-109.
- Fournie P, Touboul D, Arne JL, Colin J, Malecaze F. Keratoconus. J Fr Ophtalmol. 2013; 36(7): 618-26.
- Ahmed F, House RJ, Feldman BH. Corneal Abrasions and Corneal Foreign Bodies. Prim Care. 2015 Sep; 42(3): 363-75.
- Remington, Lee Ann. Clinical Anatomy and Physiology of The Visual System, 3rd Edition. Butterworth-Heinemann, 2012.
- Cassel GH, Billig MD, and Randall, HG. The Eye Book: A Complete Guide to Eye Disorders And Health. The Johns Hopkins University Press, 1998.