- Barbiturates are CNS depressants which were popular hypnotic and sedative of past century upto 1960s. However, their use to promote sleep or calm patient had declined in past years.
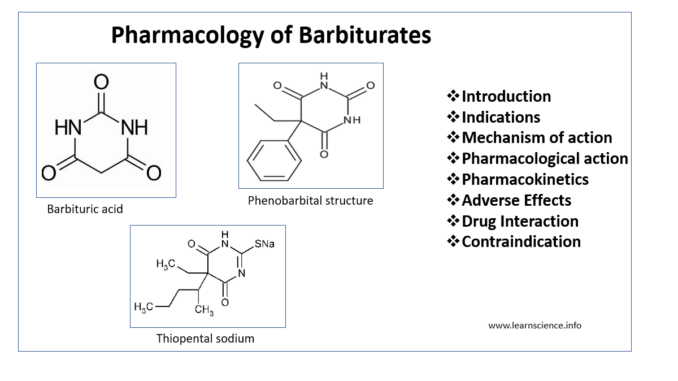
- Barbiturates are derivative of barbituric acid which is formed from malonic acid and urea. The parent compound barbituric acid was first synthesized in 1864. The first pharmacologically active agent barbital was synthesized in 1881 and introduced in medical practice in 1904. The most widely used compound phenobarbital was synthesized in 1911 and used clinically the following year.
Classification of Barbiturates
- They can be classified into 4 groups based on their duration of action. They are as follows:
- Long-acting (8 hours or more)– e.g. Phenobarbitone
- Intermediate acting (4-8 hours)– e.g. Pentobarbitone, Amylobarbitone
- Short acting (less than 4 hours)– e.g. Secobarbitone
- Ultra-short acting (in minutes)– e.g. Thiopentone
Indications
- Most of the barbiturates use have been replaced by benzodiazepines as barbiturates induce tolerance, drug dependence and serious drug withdrawal symptoms.
- Used as anti-convulsant. Phenobarbital is used in long term management of tonic- clonic seizures
- Ultra-short acting barbiturates are used to induce general anesthesia.
- Used as mild sedative to relieve anxiety, insomnia and nervous tension. Their use as hypnotics is no more recommended.
- Amylobarbitone, thiopental sodium and pentobarbitone can be used for narcoanalysis.
- Phenobarbitone is used to treat certain type of neonatal jaundice.
Mechanism of action
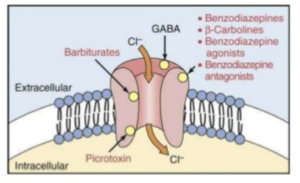
Figure – Binding site of barbiturates and their mechanism of action
- Barbiturates bind to beta-subunit of inhibitory GABAA receptor. Their binding site is distinct from benzodiazepines.
- Barbiturates prolong the opening of chloride channel increasing the chloride ion concentration in neuron. This causes hyperpolarization of neuronal membrane and makes difficult for excitatory neurotransmitters to depolarize the cell. They enhance effectiveness of GABA by lowering concentration of GABA required for opening chloride channels.
- Barbiturates can block excitatory glutamate receptors. In anesthetic concentration, pentobarbitone blocks high frequency sodium channels. These all lead to decreased neuronal activity.
Pharmacological actions
CNS actions
- Barbiturates depress the CNS in dose dependent manner. At low dose, they produce sedation and reduce excitement. At higher dose, they act as hypnotic followed by anesthesia and finally coma and death. In old people and children, they can produce excitement or dysphoria and state of confusion.
- They also possess anesthetic and anti-convulsant action.
Respiration
- They cause dose-dependent depression of respiratory center by suppressing hypoxic and chemoreceptor response to CO2. Overdose may also cause death by direct paralysis of medullary center.
Cardiovascular center
- In toxic dose, they cause hypoxia and direct depression of myocardium and vasomotor center leading to sustained hypotension.
Liver
- In acute administration, barbiturate may inhibit metabolism of certain drugs and endogenous steroids by combining with various CYP450 enzymes. Chronic administration may cause induction of hepatic microsomal enzymes resulting in increased inactivation of certain drugs.
- Phenobarbitone stimulate the metabolism of bilirubin.
Pharmacokinetics
- They are well absorbed after oral administration. As they are weak acid, maximum absorption occurs from stomach where they exist in unionized from. Absorption also occurs from the intestine and rectum. IV route is preferred for anti-epileptic and anesthetic action. IM route is also used.
- They are distributed in all tissues and body fluids. The distribution depends on factors like lipid solubility, extent of ionization and degree of protein binding. Highly lipid soluble barbiturates like thiopental sodium undergoes redistribution form CNS to less vascularized tissues, especially fat and muscle. This movement is responsible for their short duration of action.
- They can cross placental barrier and are secreted in milk.
- They are metabolized in liver and inactive metabolites are excreted in urine.
Adverse effects
- Barbiturates cause drowsiness, impaired concentration and mental and physical sluggishness. Hypnotic dose is associated with hangover symptom characterized by drowsiness, dysphoria and motor depression.
- Allergic reaction includes urticaria, edema, agranulocytosis and thrombocytopenic purpura.
- Repeated administration of barbiturate cause tolerance to their sedative and hypnotic actions. It also causes drug dependence.
- Abrupt withdrawal from barbiturates is severe and may cause nausea, vomiting, tremor, weakness, restlessness, delirium and cardiac arrest.
- Barbiturate may precipitate attack of acute intermittent porphyria. Prolonged phenobarbitone therapy may cause megaloblastic anemia.
- Drug automatism- Patient using barbiturate as hypnotic, may repeatedly take barbiturate at night due to confusion and amnesia and poison himself. This phenomenon is called drug automatism.
- Overdose may lead to acute barbiturate poisoning which is life-threatening.
Drug Interaction
- Barbiturates induce hepatic microsomal enzyme and may decrease effectiveness of drugs like ritonavir, voriconazole, oral anticoagulants like warfarin, thyroxine, phenytoin, chloramphenicol, griseofulvin and theophylline.
- Concurrent use with other CNS depressants like alcohol, benzodiazepines, antihistamines and MAO inhibitor may result in severe CNS depression.
Contraindication
- Contraindicated in patients with acute intermittent porphyria.
- Contraindicated in patients with known hypersensitivity to barbiturates.
- They are avoided in pregnancy and nursing mothers.
References
- Ernst BJ, Clark GF, Grundmann O. The Physicochemical and Pharmacokinetic Relationships of Barbiturates – From the Past to the Future. Curr Pharm Des. 2015; 21(25): 3681-91.
- Ito T, Suzuki T, Wellman SE, Ho IK. Pharmacology of barbiturate tolerance/dependence: GABAa receptors and molecular aspects. Life Sciences. 1996; 59(3): 169-195.
- https://www.britannica.com/science/barbiturate
- https://www.emcdda.europa.eu/publications/drug-profiles/barbiturates_en
- https://www.medicinenet.com/barbiturates-oral/article.htm#what_about_taking_barbiturates_during_pregnancy_or_while_breastfeeding
- Pharmacology and Pharmacotherapeutics book. 24th edition
- Goodman and Gillman’s Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology. 6th edition.