- Allopurinol is xanthine oxidase inhibitor used in treating gout. Chemically, it is 4-hydroxy-pyrazolo 3, 4 d-pyrimidine. It is an analogue of hypoxanthine.
- It was approved for its medical use by FDA in 1966.
Indications of Allopurinol
- Gout– Used in long term management of gout. It is effective for treating primary hyperuricemia (increased uric acid level) of gout. Gout is a disease characterized by deposition of monosodium urate crystals inn body tissues, especially around joints.
- Secondary hyperuricemia– Used in hyperuricemia which may occur following the use of cytotoxic drugs while treating leukemia and lymphoma. Allopurinol is started before starting the chemotherapy and should be stopped when chances of overproduction of uric acid is not present.
- Used in prevention of tumor lysis syndrome and prevention of recurrent calcium nephrolithiasis in patients with hyperuricosuria.
- Non-FDA indications include Lesch- Nyhan syndrome associated hyperuricemia and prevention of recurrent uric acid nephrolithiasis.
Mechanism of action of Allopurinol
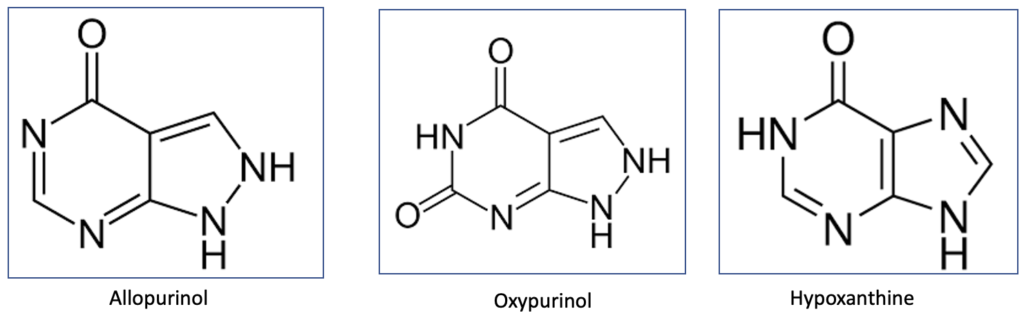
Figure- Structure of allopurinol, oxypurinol and hypoxanthine
- Allopurinol is structural analogue of natural purine base, hypoxanthine and is xanthine oxidase inhibitor. Its metabolite, oxypurinol (alloxanthine) is also active xanthine oxidase inhibitor.
- Purine nucleotides during purine metabolism are degraded to hypoxanthine and xanthine, which are oxidized to uric acid by xanthine oxidase. Allopurinol and alloxanthine inhibit xanthine oxidase and hence, inhibit formation of uric acid from hypoxanthine and xanthine. Hence, the concentration of uric acid in plasma decreases and purine excretion is increased without exposing urinary tract to excessive load of uric acid leading to decrease in incidence of gout symptoms.
- Allopurinol treatment may increase concentration of xanthine and hypoxanthine. However, both compounds are more soluble and can be excreted rapidly by kidneys which prevent the risk of their crystallization in kidneys and other tissues.
Pharmacokinetics of allopurinol
- It is absorbed rapidly after oral administration. Peak plasma concentration is achieved within 60-90 minutes of oral administration. It is also administered via IV route.
- It is metabolized in liver to oxypurinol which is a weak xanthine oxidase inhibitor. Oxypurinol is detected in circulation within 15 minutes of allopurinol administration. Oxypurinol concentration is higher than that of parent drug. Plasma half-life of allopurinol is 1-2 hours and of oxypurinol is 18-30 hours. The long half-life of oxypurinol allows for once daily dosing of allopurinol. Both allopurinol and oxypurinol are distributed in total tissue water and are not bound to plasma proteins.
- About 20% of administered drug is excreted via feces in unabsorbed form and 10-30% is excreted unchanged in urine. Remaining is metabolized to oxypurinol which is excreted slowly via urine.
Adverse effects
- It is tolerated well by most of the patients. Adverse effects occur in around 15-20 % of the patients.
- Common adverse effects include hypersensitivity reactions, especially skin rashes. This risk is more in patients with impaired renal function. Hypersensitivity reactions can be mild to life-threatening and include Steven-Johnson syndrome.
- During the first few months after starting allopurinol therapy, acute attacks of gout may occur due to mobilization of tissue stores of uric acid. Hence, colchicine is administered to suppress such acute attacks.
- Other side effects include nausea, vomiting, diarrhea, hepatic damage, and vasculitis. It can also cause transient leukopenia and eosinophilia which require cessation of therapy.
Drug Interaction
- It interferes with metabolism of drugs like 6-mercaptopurine, azathioprine and theophylline. Hence, when these drugs are co-administered with allopurinol, dosage of these drugs should be reduced.
- It may interfere with hepatic inactivation of warfarin. Patients receiving both medicines should be continuously monitored for prothrombin activity.
- It may increase half-life of probenecid and increase its uricosuric activity. Probenecid may increase excretion of oxypurinol.
Contraindications
- Contraindicated in patients hypersensitive to allopurinol.
References
- https://go.drugbank.com/drugs/DB00437
- https://www.ncbi.nlm.nih.gov/books/NBK499942/
- Turnheim K et al. Pharmacokinetics and pharmacodynamics of allopurinol in elderly and young subjects. Br J Clin Pharmacol. 1999 Oct; 48(4): 501–509.
- Murrell GAC et al. Clinical Pharmacokinetics of Allopurinol. ClinicalPharmacokinetics. 1986; 11:343–353.
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- Essentials of Medical Pharmacology. 7th edition.