- Antibiotics are the most commonly prescribed medicines across all over the world. Penicillin is among the most important antibiotics, which belong to group beta-lactam antibiotics. Penicillin is effective at eradicating common bacterial infections and are inexpensive, so it is widely prescribed to treat ear, skin, sinus and urinary tract infection.
- Like other drugs, penicillin also have some adverse effects. Hypersensitivity or allergic reactions is one of the complications of penicillin therapy observed in 0.7-4% of cases.
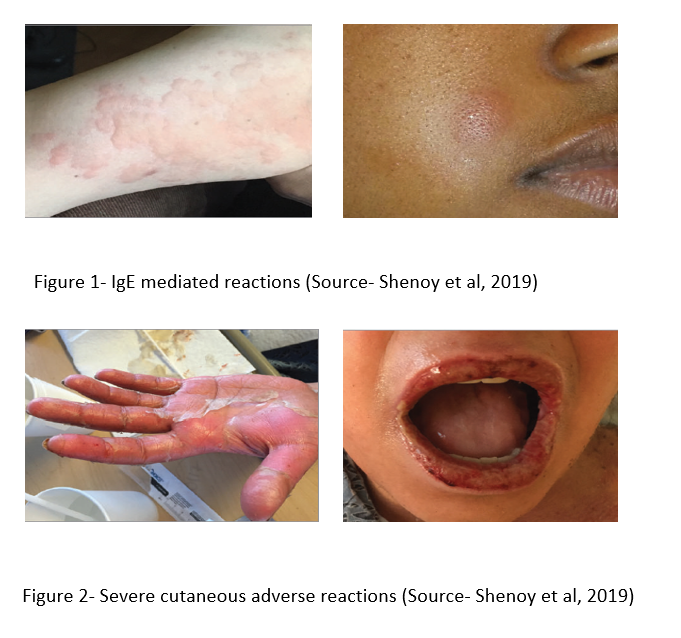
- All types of natural and semi-synthetic penicillin show allergic reactions. There are two clinical features of penicillin allergy; acute and sub-acute. The acute allergic reaction occurs immediately within minutes or hours of penicillin administration and is characterized by sudden anaphylaxis with hypotension, urticaria and bronchospasm. It is mediated by IgE antibodies.
- The sub-acute reaction may occur 7-10 days after starting of penicillin therapy or 1-2 days after repeat therapy. The signs are similar as in acute phase and is mediated by IgG antibodies.
- It is mostly seen after parenteral or topical administration of penicillin than oral administration. Procaine penicillin has high chances of causing allergy as procaine itself is allergenic.
- The hypersensitivity caused by penicillin is unpredictable. The person who can tolerate initial dose of penicillin may show allergic symptoms on subsequent administration and vice-versa.
The important allergic reactions are-
- Skin rashes: of various types associated with pruritus. Contact dermatitis may occur in pharmacists, nurses and clinicians who prepare penicillin solutions.
- A serum sickness like syndrome: characterized by rash, fever, bronchospasm, arthralgia and eosinophilia. Fever disappears within 24-36 hours after cessation of drug administration but may persist for days.
- Renal disturbances: like hematuria and albuminuria.
- Hemopoietic disturbances: like hemolytic anemia and neutropenia (rare).
- Anaphylaxis: most serious reaction but occurs in fewer than 0.01 % of patients. The symptoms begin within few minutes of penicillin administration and is characterized by bronchospasm, angioedema and acute cardiovascular collapse
Mechanism of Penicillin Allergy
- Penicillin and its metabolites form covalent bond with proteins present in serum and tissues and act as haptens. The beta-lactam ring while binding to lysine residues in serum proteins, creates penicilloyl polylysine which is major antigenic determinant. Haptenation from covalent bonding create several minor determinants.
- The hapten-pro hapten model applies to immediate or antibody mediated penicillin hypersensitivity.
- Delayed reactions are associated with model that involves non-covalent binding.
Tests for detection of Penicillin Allergy
- A reliable method to detect penicillin allergy is not available till date. History of allergy or positive skin test is not complete evidence of allergy. Similarly, negative skin test and negative history of allergy doesn’t completely indicate safety of penicillin administration.
- Skin tests can be done by scratching the skin through a drop of solution containing 10,000 units of benzylpenicillin per ml or by intradermal administration of 0.05 ml of peniclloyl-polylysine or by combining both.
- Persons with a history of penicillin allergy and negative result in skin test have no greater risk of rashes associated with penicillin antibiotics.
- Unfortunately, in some cases fatal anaphylactic reactions may occur even in persons with negative skin response and some persons with positive skin reactions have accepted penicillin without serious reactions. In some cases, even the small amount of penicillin used for test may cause severe reactions.
Management of patient potentially allergic to Penicillin
- The most efficient way to identify patients at risk of penicillin allergy is to evaluate their history. Skin test is also effective. Most patients with a history of penicillin allergy should be treated with other antibiotics.
- An individual allergic to one type of penicillin should not be administered other types of penicillin.
- If penicillin-allergic patients must receive the drug, penicillin desensitization should be carried out. This is done by administering increasing dose of penicillin in the hope of binding all IgE without provoking anaphylaxis. After reaching the full dose, penicillin should not be stopped and then restarted as immediate allergic reaction may occur. This method should be carried out only in an intensive care setting and its efficacy is unproven.
Drug therapy and emergency medical care
- A mild allergic reaction can be treated with antihistamines which helps to relieve rashes and itching.
- Serious anaphylactic reactions should be treated by administering adrenaline and glucocorticoids. Adrenaline helps to counter cardiac collapse and glucocorticoids help to counter effects of mediators released from mast cells.
References
- Bhattacharya S. The facts About Penicillin Allergy. J Adv Pharm Technol Res. 2010 Jan-Mar; 1(1): 11–17.
- Shenoy ES, Macy E, Rowe T, Blumenthal KG. Evaluation and Management of Penicillin Allergy A Review. JAMA. 2019; 321(2): 188-199.
- Castelles M, Khan DA, Philips EJ. Penicillin Allergy. N Engl J Med. 2019; 381(24): 2338-2351.
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.