- Antiarrhythmic drugs are used to treat abnormal heart rhythm. These drugs are classified based on Vaugha-Williams classification:
- Class I (fast sodium channel blocker)
- Class II (beta adrenergic blocker)
- Class III (potassium channel blocker)
- Class IV (Calcium channel blocker)
- Class V (miscellaneous)
- Class I antiarrhythmic drugs are again classified into IA, IB and IC on basis of their impact on length of action potential.
- Class IB antiarrhythmic drugs are those which weakly block sodium channel and decrease action potential duration.
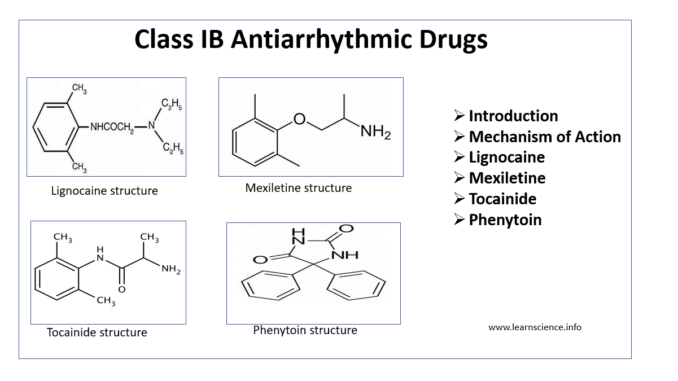
- Drugs belonging to this class are lignocaine, phenytoin, tocainide and mexiletine.
Mechanism of Action of Class IB Anti-arrhythmic Drugs
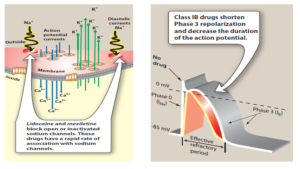
Figure 1- Schematic representation of effects of class IB anti-arrhythmic agents (source- Lippincott’s Illustrated Reviews)
- They weakly block sodium channel, shorten phase 3 repolarization and decrease action potential duration.
- They suppress automaticity and have very less effect on conduction velocity.
Explanation of individual drug of Class IB Anti-arrhythmic Drugs
Lignocaine
- Lignocaine is amide type local anesthetic and is also included in list of World Health Organization’s essential drugs list. It is also known as lidocaine.
Pharmacological effects
- It blocks both open and inactivated cardiac Na+ When given through IV route, it shortens ventricular action potential, selectively act on diseased or ischemic myocardium, depress diastolic depolarization and automaticity in ventricular tissues.
- It has little influence on conduction velocity, doesn’t affect electrophysiological functions of atria, SA node and AV node and has no hemodynamic adverse effects.
Pharmacokinetics
- IV route is preferred over oral route as it undergoes extensive first pass hepatic metabolism. Its metabolites glycine xylidide (GX) and monoethyl GX are less potent than lignocaine.
- It binds to plasma protein (60-80%) and its half life is 15-30 minutes after single injection.
- When given in combination with drugs which affect CYP isoenzymes, it should be monitored closely.
Adverse Effects
- It is relatively safe drug.
- Adverse effects include drowsiness, muscle twitching, blurred vision, confusion and convulsion.
Use
- Most useful in abolishing ventricular arrhythmia.
- As it doesn’t affect AV nodal conduction velocity, it is used for treating digitalis induce ventricular arrhythmia.
- Emergency termination of ventricular tachycardia following recent MI (Myocardial Infarction) and occurring during cardiac surgery.
Mexiletine
- It is chemical analogue of lignocaine and thus is pharmacologically similar to lignocaine. However, it is effective as oral formulation (it doesn’t undergo first-pass hepatic metabolism).
- It has narrow therapeutic index. Common adverse effects are tremor, nausea, vomiting, ataxia, blurred vision and hypotension.
- Mexiletine is approved for treating ventricular arrhythmia. It is used in combination with quinidine or sotalol may increase efficacy and reduce side effects.
Tocainide
- It is an amine analogue of lignocaine and can be used orally for treating ventricular arrhythmia. It is also reported to be effective in trigeminal neuralgia, tinnitus.
- Due to its serious adverse reactions including neurological adverse effects and aplastic anemia, its use is discontinued nowadays. However, its various analogues have been developed as sodium channel inhibitors.
Phenytoin
- Phenytoin is commonly used anti-epileptic drug.
- Phenytoin is mainly used to treat digitalis induced cardiac arrhythmia. It is also useful in prevention of recurring cardiac arrhythmias.
- It is mainly used when other agents are contraindicated or unavailable.
- Phenytoin was popularly used as antiarrhythmic drug from 1950s to 1970s. Its use as antiarrhythmic drug has lessen in recent decades due to introduction of newer and less toxic agents.
- It is administered through oral or slow IV route.
References
- Weinberg L, Peake B, Tan C, Nikfarjam M. Pharmacokinetics and pharmacodynamics of lignocaine: A review. World J anesthesiol. 2015; 4(2):17-29.
- Meyler’s Side Effects of Drugs (Sixteenth Edition). The International Encyclopedia of Adverse Drug Reactions and Interactions. 2016; Pages 36-38.
- Nerves and Nerve Injuries Vol 2: Pain, Treatment, Injury, Disease and Future Directions. 2015; Pages 81-97.
- Karthikeyan M. Therapeutic Applications of Phenytoin. Asian Journal of Pharmaceutical and Clinical Research. 2009; 2(3):1-14.
- Wang LW, Subbiah RN, Kilborn MJ, Dunn RF. Phenytoin: an old but effective antiarrhythmic agent for the suppression of ventricular tachycardia. Med J Aust. 2013; 199 (3): 209-211.
- https://www.amboss.com/us/knowledge/Antiarrhythmic_drugs
- Pharmacology and pharmacotherapeutics. 24th edition.
- Goodman and Gillman’s Manual of Pharmacology.
- Lippincott’s Illustrated Reviews. 6th edition.