- Spiramycin is a member of macrolide antibiotic. Macrolide antibiotics are a group of antibiotics which are composed of a macrocyclic lactone of different ring sizes to which one or more deoxy sugars are attached. The ring is either 14, 15 or 16 membered.
- Spiramycin has 16 membered rings. It was discovered in 1952 and is produced by Streptomyces ambofaciens. It is similar to erythromycin in properties and activity spectrum.
- Spiramycin is not commercially available in United States.
Indications of spiromycin
- It is mainly used to treat acute acquired toxoplasmosis in pregnancy to prevent transmission to fetus. It gets concentrated in plasma and is found to reduce transmission by 60%.
- Used for various other bacterial infections including whooping cough, cryptosporidiosis, tonsilitis, pharyngitis. However, it’s uses for this purpose is less common due to availability of other alternative agents.
Antibacterial spectrum of spiramycin
- It has bacteriostatic effect mainly against gram- positive cocci and rods. It is also effective against gram- negative cocci, Legionellae, Toxoplasma gondii, some type of spirochetes and Cryptosporidium.
Mechanism of action of spiramycin
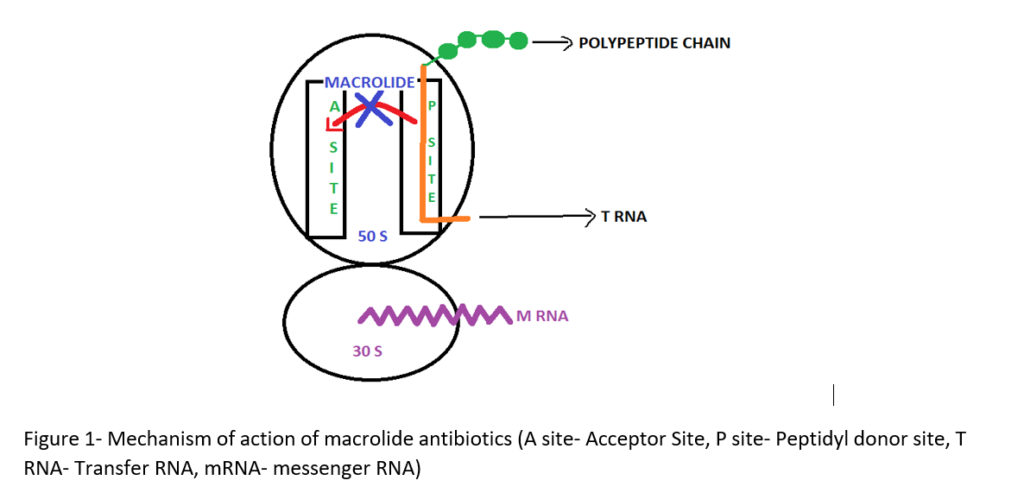
- Its mechanism of action is similar to other macrolide antibiotics. It binds irreversibly to 50S ribosomal subunit of bacteria with apparent 1:1 stoichiometry and inhibit translocation step of protein synthesis. In translocation step a newly synthesized peptidyl tRNA molecule moves from the acceptor site on the ribosome to the peptidyl donor site.
- It mainly stimulates dissociation of peptidyl t-RNA from ribosomes during translocation.
Pharmacokinetics of spiramycin
- Oral spiramycin is generally well tolerated and shows good bioavailability (30- 50%). Administration with food may reduce its bioavailability by around 50%. It is also administered through rectal or parenteral route. It is available as tablet, capsule and IV formulation.
- Its half-life after oral administration is 5.5- 8 hours. Although it gets concentrated in placenta, it cannot cross the placenta and reach to fetus. It is secreted in milk.
- It doesn’t cross blood brain barrier and reach in CSF (cerebrospinal fluid). Hence, it should not be used to treat Toxoplasma encephalitis.
Adverse effects
- It is generally well tolerated drug. GI distress is major effect when given through oral route. Some common adverse effects include rashes, diarrhea, nausea and vomiting.
- Some other reported side effects include cholestatic hepatitis, thrombocytopenia, pseudomembranous colitis, oxidative hemolysis in patients with glucose-6- phosphate dehydrogenase deficiency.
Drug Interaction
- Some medicines that may interact with spiramycin include ergot alkaloids, dihydroergotamine, methysergide and levomethadyl. Hence, the coadministration of spiramycin and these drugs is not recommended.
- It prolongs elimination half-life life of levodopa and carbidopa resulting in increased risk of some side effects. When co-administration of spiramycin and these agents is required, dose adjustment should be done.
Contraindications
- It should be used with caution in patients with known history of hypersensitivity to macrolide antibiotics.
- Used with caution in hepatic impairment.
- It is pregnancy category B drug which means it is safe to use in pregnancy.
References
- Zeid et al. Spiramycin, a macrolide antibiotic. Zentralbl Bakteriol Naturwiss. 1980;135(5):443-53.
- https://go.drugbank.com/drugs/DB06145
- https://www.mayoclinic.org/drugs-supplements/spiramycin-oral-route-injection-route-rectal-route/side-effects/drg-20066104?p=1
- Infectious Diseases (Fourth Edition). 2017; 2: 1345-1372.e2.
- Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases (Eighth Edition). 2015; 1; 510-518.e3.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Pharmacology and Pharmacotherapeutics book. 24th edition.
- Essentials of Medical Pharmacology. 7th edition.