- Morphine is widely used opium alkaloid to treat moderate to severe pain. It remains as standard against which newly discovered analgesics are compared.
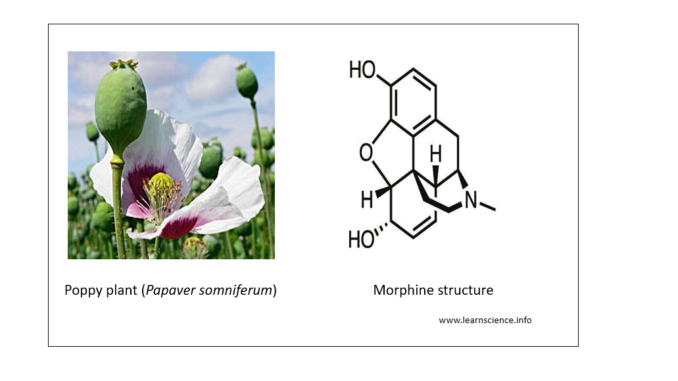
- Morphine is extracted from dried milky exudate of unripe seed capsule of the opium poppy. It occurs as colorless crystals or white crystalline powder.
- It was first isolated from opium by German scientist F.W.A Serturner in about 1804 after which true modern opioid pharmacology begins. There is also some evidence that the opium poppy plant ‘Papaver somniferum’ was also cultivated for its active ingredients as early as 3000 BC.
- Derivatives of morphine includes codeine, dihydrocodeine, ethyl morphine, heroine and dihydromorphine.
Mechanism of action of morphine
- Morphine acts on mu (µ) receptors (a kind of opioid receptors) present in CNS and other tissues. Other opioid receptors are kappa, delta and nociceptin receptors. Mu receptors are found mainly in brainstem and medial thalamus. Subtypes are Mu1 and Mu2 with Mu1 related to analgesia, euphoria and Mu2 related to respiratory depression, release of prolactin and anorexia.
- After binding to µ receptors, morphine blocks transmission of nociceptive signals and inhibit transmission from primary afferent nociceptors to dorsal horn sensory projection cells.

Pharmacokinetics of Morphine
- It can be given through oral, intravenous, intramuscular and subcutaneous route. It is metabolized during first pass though the liver, so oral bioavailability is about 20-40 %. When used orally, it is used in an extended release form.
- It circulates in plasma partly in free form and partly in protein-bound form. It rapidly enters all body tissues. Also it enters the brain rapidly, can cross placental barrier and is also secreted in milk.
- It is metabolized in liver and kidney by combination with glucuronic acid, oxidation and N-dealkylation. Its metabolite morphine-6-glucuronide has analgesic properties and is more potent than morphine.
- Morphine has short half-life of around 2.5-3 hours and morphine-6-glucuronide has half life of around 2 hours.
- Around 90 % is excreted through urine and 7-10 % in the form of biliary excretion.
- Special population including infants, elder people and hepatic or renal patient have a unique morphine pharmacokinetic profile which must be considered before administering morphine to maximize efficacy and reduce adverse effects.
Clinical uses of Morphine
- For relieving pain. The effective dose is highly variable. It is usually administered via IV route for relieving sudden pain. It can be used for relief of pain in renal and biliary colic in combination with atropine. Morphine is also effective in treating cancer pain, and post-operative pain.
- In treating acute left ventricular failure and pulmonary edema.
- As pre-anesthetic medication.
- In diarrhea (rarely).
- As an anesthetic either alone or in combination to produce general anesthesia in person who are considered as bad anesthetic risks.
- As sedative in threatened abortion.
- In acute coronary syndrome.
Adverse effects
- Respiratory depression occurs even in small doses. Patients should be monitored for respiratory depression especially within first 24-72 hours of initiating therapy and with all dose increases.
- Allergic skin rashes, contact dermatitis, pruritus may occur due to release of histamine. Anaphylactoid reaction with fall in BP are reported.
- It may cause nausea, vomiting, mental clouding, dysphoria, headache and fatigue. It also causes constipation, hypotension and urinary retention.
- Tolerance and drug dependence are major drawback of morphine therapy. Repeated administration may develop tolerance. Physical and psychological dependence may occur. Withdrawal symptoms include fever, increase in heart rate and BP, intestinal cramps, insomnia, weakness and back and leg pain for several weeks.
To prevent it’s dependence, it should not be prescribed for chronic pain except in cases of terminal cancer pain.
- When it is administered to mother during labor can depress fetal respiration.
Precaution with morphine therapy
- Old people and infants are more prone to develop respiratory depression so, it should be used with care in such population. Even in patients with hepatic or renal impairment, extra caution is necessary.
- It should be administered with caution in patients with decreased respiratory reserve like in emphysema, COPD (Chronic Obstructive Pulmonary Disease). In COPD patients, even therapeutic doses of morphine may produce death.
- It should be avoided in patients with head injuries as it causes increase in CSF pressure, stimulate spinal cord and produce respiratory depression.
Preparations and dosage
- Controlled release tablets (10, 30 and 60 mg) of morphine sulfate for prolonged action.
- Morphine solution (2-20 mg/ml) for oral use. Dose in adults is 10-30 mg. Larger doses (up to 200 mg) are needed in patients with terminal cancer. Orally, it is only about one sixth as effective as parenteral administration.
- Morphine hydrochloride or sulfate injection. Dose: 10-20 mg SC or IM; 2.5-5 mg IV over 5 minutes. It has also been used by a continuous, low dose, IV infusion by epidural and intrathecal administration. If given by IV infusion, 10 mg are infused over the first 1 hour and 10 mg over the next 4 hours.
References
- Sverrisdóttir E, Lund TM, Olesen AE, Drewes AM, Christrup LL, Kreilgaard M. A review of morphine and morphine-6-glucuronide’s pharmacokinetic-pharmacodynamic relationships in experimental and clinical pain.Eur J Pharm Sci. 2015 Jul 10; 74: 45-62.
- Lugo RA. Clinical Pharmacokinetics of Morphine. Journal of Pain and Palliative Care Pharmacotherapy. 2002; 16(4): 5-18.
- Pacifici GM. Metabolism and pharmacokinetics of morphine in neonates: A review. Clinics (Sao Paulo). 2016 Aug; 71(8): 474–480.
- Trescot AM, Datta S, Lee M, Hansen H. Opioid Pharmacology. Pain Physician. 2008; 11: S133-S153.
- Pathan H, Williams J. Basic opioid pharmacology: an update. Br J Pain. 2012 Feb; 6(1): 11–16.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- Pharmacology and pharmacotherapeutics. 24th edition.
- A Textbook of Clinical Pharmacology and Therapeutics. 5th edition.