- Macrolide antibiotics are a group of antibiotics which are composed of a macrocyclic lactone of different ring sizes to which one or more deoxy sugars are attached. The ring is either 14, 15 or 16 membered.
- Currently available macrolide antibiotics are:
- Erythromycin
- Clarithromycin
- Azithromycin
- Fidaxomicin
- Telithromycin.
- Telithromycin is related ketolide. Among these, erythromycin was isolated from Streptomyces erythreus in 1952 whereas others are semi-synthetic derivatives.
- All macrolide antibiotics have broad spectrum of activity against many gram-positive bacteria. Fidaxomicin is narrow spectrum macrolide.
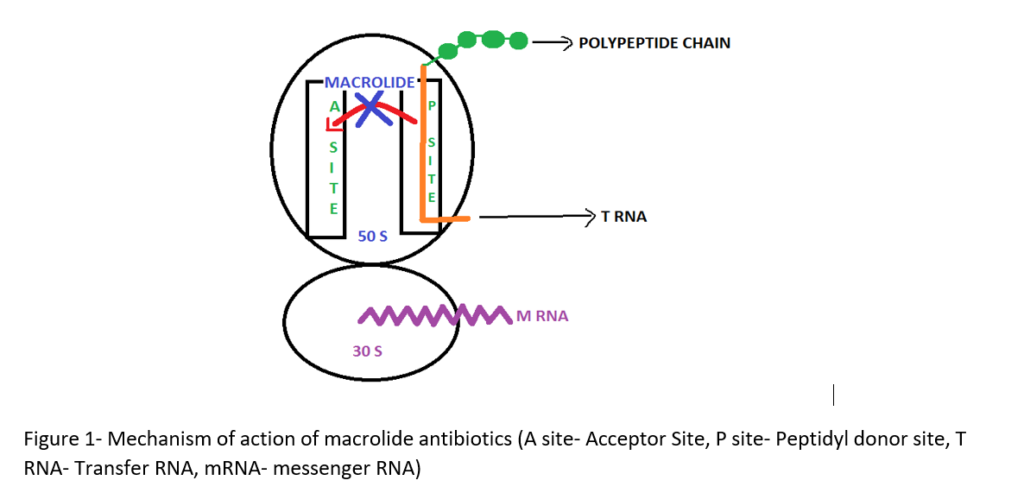
Mechanism of action of macrolide antibiotics
- It binds irreversibly to 50S ribosomal subunit of bacteria and inhibit translocation step of protein synthesis. In translocation step a newly synthesized peptidyl tRNA molecule moves from the acceptor site on the ribosome to the peptidyl donor site. It also inhibits other steps like transpeptidation.
- Depending on its concentration, it can be bactericidal or bacteriostatic.
- Mechanism of action of fidaxomicin is quite unique. It acts on the sigma subunit of RNA polymerase, disrupt bacterial transcription resulting in termination of protein synthesis and cell death in susceptible organisms.
Antibacterial spectrum of macrolide antibiotics
- They are active mainly against Gram‐positive bacteria and have limited activity against Gram‐negative bacteria.
- Macrolides are very active against Staphylococcus, Streptococcus and Diplococcus Gram‐positive bacteria, and among Gram‐negative cocci, Neisseria gonorrhoea, Haemophilus influenzae, Bordetella pertussis and Neisseria meningitis. Additionally, they are also extremely active against various Mycoplasmas.
Pharmacokinetics of macrolide antibiotics
Absorption:
- They are adequately absorbed upon oral administration. Erythromycin and azithromycin are available in IV formulations also.
- The erythromycin base is inactivated by gastric acid, so it is administered in form of either enteric-coated tablets, as capsules containing enteric coated pellets or esterified forms. Clarithromycin, azithromycin, and telithromycin are stable in stomach acid and are readily absorbed.
- Food interferes with the absorption of erythromycin and azithromycin but can increase that of clarithromycin. The extended form of clarithromycin is given along with food to increase its bioavailability.
Distribution:
- Erythromycin diffuses readily into intracellular fluids except the brain and CSF (Cerebrospinal Fluid). It crosses placenta and is also secreted in milk.
- Clarithromycin, azithromycin, and telithromycin are widely distributed in the tissues. Fidaxomicin remains locally confined to and act in the gut after oral administration.
- Azithromycin’s unique pharmacokinetic properties include extensive tissue distribution and high drug concentrations within cells (including phagocytes), resulting in much greater concentrations of drugs in tissue or secretions compared to simultaneous serum concentrations. It has the longest half-life and largest volume of distribution among all.
Elimination
- Erythromycin and telithromycin are extensively metabolized hepatically.
- Erythromycin and azithromycin are primarily concentrated and excreted in the bile as active drugs. Partial reabsorption occurs through the enterohepatic circulation. Clarithromycin and its metabolites are eliminated by the kidney as well as the liver. The dosage of this drug should be adjusted in patients with renal impairment.
- Fidaxomicin is metabolized by CYP isoenzymes and primarily excreted through fecus. Less than 1 % is excreted as urine.
Clinical Uses
- Used as alternative for treatment of patients who are allergic or resistant to penicillin.
- In mycoplasma pneumonia and in chlamydial infection.
- In whooping cough caused by B. pertussis.
- Used in legionella infection and in diphtheria.
- Clarithromycin is used in combination therapy with omeprazole and amoxicillin to treat H. pylori infection.
- To treat Campylobacter gastroenteritis in children.
- In tetanus.
- Fidaxomicin is used to treat diarrhea caused by infection with Clostridium difficile.
Adverse Effects
- Allergic reaction like rashes, fever, eosinophilia may occur which resolve after therapy is stopped.
- Gastric upset is most common adverse effect (primarily in erythromycin). Azithromycin and clarithromycin are better tolerated.
- Cholestatic jaundice is serious side effect of caused primarily by erythromycin estolate. It starts after 1-3 weeks of treatment and is associated with abdominal cramp, vomiting, jaundice, fever and leukocytosis.
- Telithromycin use is restricted due to its severe irreversible hepatotoxicity named ‘Ketek effects’.
- High doses of erythromycin may cause transient deafness. Azithromycin is also associated with irreversible sensorineural hearing loss.
Contraindications
- Erythromycin, azithromycin and telithromycin should be used with caution in patients with hepatic dysfunction as they get accumulated in liver.
- Macrolides should be used with caution in proarrhythmic patients or those who are taking proarrhythmic medicines.
Drug Interactions
- Erythromycin, telithromycin, and clarithromycin inhibit the hepatic metabolism of several drugs, which can lead to toxic accumulation of these compounds. Such drugs are atorvastatin, carbamazepine, simvastatin, valproate, theophylline and protease inhibitors.
Resistance
- Resistance may be due to:
- ribosomal protection by methylase enzymes that modify ribosomal target and decrease drug binding.
- chromosomal mutations that alter a 50S ribosomal protein (found in B. subtilis, Campylobacter spp., mycobacteria, and gram-positive cocci).
- macrolide hydrolysis by esterase produced by Enterobacteriaceae.
- drug efflux by active pump mechanism.
- Inability of organism to take up the antibiotic.
- Resistance to erythromycin has been increasing, resulting in its limited clinical use (particularly for S. pneumoniae). Both clarithromycin and azithromycin share some cross-resistance with erythromycin, but telithromycin may be effective against macrolide resistance organisms.
References
- https://www.drugs.com/mtm/fidaxomicin.html
- https://www.ncbi.nlm.nih.gov/books/NBK548398/
- Laslop NV, Mankin AS. How Macrolide Antibiotics Work. Trends Biochem Sci Actions. 2018; 43(9): 668-684.
- Fernandes P, Martens E, Pereira D. Nature Nurtures the Design of New Semi-Synthetic Macrolide Antibiotics. J Antibiot. 2017; 70(5): 527-533.
- Dinos GP. The macrolide antibiotic renaissance. British Journal of Pharmacology. 2017; 174: 2967- 2983.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
Very detailed information thanks