- Heparin is earliest and most widely used anticoagulant and antithrombotic drug which is still in use nowadays. It occurs naturally in mast cells which are present in liver and lungs.
- It was first discovered in 1916 by McLean, a medical student. The name ‘heparin’ was introduced in 1918 by Howel and Holt. It was successfully used in clinical practice only in 1937.
Biochemistry of heparin
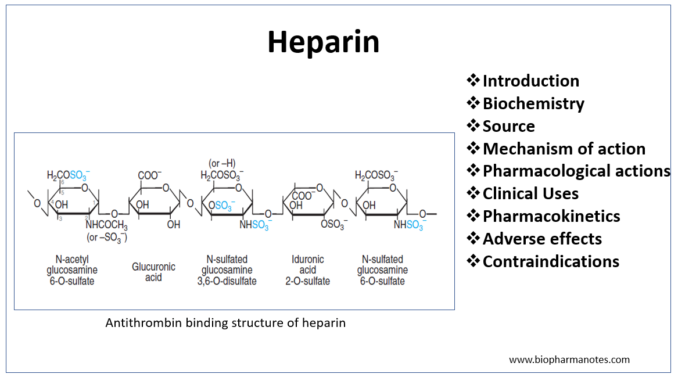
- It is a non-uniform mixture of straight chain mucopolysaccharides with wide range of molecular weight (3000- 30,000 dalton). It contains polymers of two sulfated disaccharide units: D-glucosamine-L-iduronic acid and D-glucosamine-D-glucuronic acid. The chain length and proportion of these two disaccharide units may vary.
- It has very strong electronegative charge due to presence of high concentration of esterified sulfuric acid. Hence, it is the strongest organic acid occurring in the body.
- Once it is released from mast cells, it undergoes rapid degradation by macrophages. So, it cannot be detected in normal plasma.
Source
- Heparin is extracted for medical use from porcine intestinal mucosa or bovine lung. It’s bioassay depend on its capacity to prevent clotting of cattle or sheep plasma under standardized conditions.
- Low molecular weight heparins (LMWH) are prepared by fractionation of native heparin. LMWH consist of 15-17 saccharide chains and have molecular weight of around 4000- 6500. Some examples are enoxaparin, dalteparin sodium, pamparin etc.
Mechanism of action of heparin
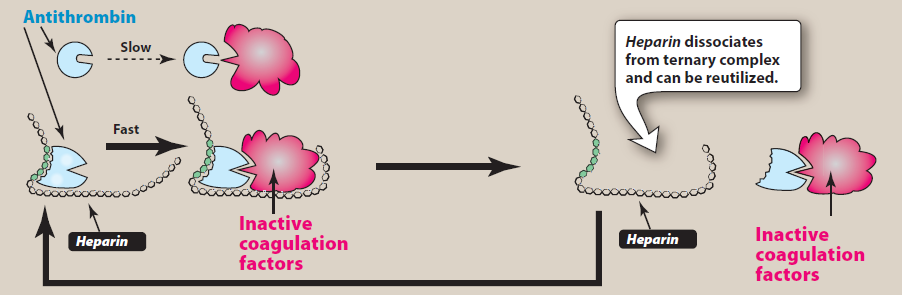
Figure- Heparin accelerates inactivation of coagulation factors by activating antithrombin (Source- Lippincott’s Illustrated Reviews, 6th edition)
- The anticoagulant action is due to its binding with antithrombin III which results in rapid inactivation of coagulation factors.
- Antithrombin III is an α globulin which inhibits serine protease of thrombin (factor IIa), IXa and Xa clotting factors. When heparin is not present, the interaction between antithrombin with these two factors is slow. In presence of heparin, antithrombin binds with heparin which lead to confirmational change and increase the interaction and inhibition of thrombin by about 1000 times. Once antithrombin is bound to thrombin, heparin molecule is released from complex.
- LMWH mainly produces their anticoagulant effect by catalyzing inhibition of factor Xa rather than thrombin.
Pharmacological action of heparin
Blood coagulation– It acts as anticoagulant both in vivo and in vitro. When used in therapeutic doses, it prolongs the clotting time and activate partial thromboplastin time.
Heparin and lipoprotein lipase– It activates lipoprotein lipase and abolishes cloudiness of hyperlipemic plasma within minutes of its administration.
Miscellaneous actions– It possess some anti-inflammatory action. It inhibits aldosterone secretion and inhibits growth of many cells like vascular muscle and endothelium in culture.
Clinical uses
- Used in treatment of acute venous thromboembolism.
- Used for prophylaxis of postoperative venous thrombosis in patients undergoing surgery and those with acute MI (Myocardial Infarction).
- It is the choice of anticoagulant drug to be used in pregnancy as it doesn’t cross placenta due to large size and negative charge. Warfarin cannot be used in pregnancy due to teratogenic effects.
- To prevent formation and extension of thrombus.
- Used in initial management of patients with unstable angina or acute MI, during and after coronary angioplasty or stent placement, and during surgery requiring cardiopulmonary bypass.
- Used to treat selected patients with disseminated intravascular coagulation.
Pharmacokinetics
- It is not well absorbed when administered through oral route. So, it is mostly administered through IV or subcutaneous route. When given through IV route, it shows immediate onset of action. Heparin is often initiated as IV bolus to achieve immediate anticoagulation which is followed by lower dose or continuous infusion of heparin.
- The half-life depends on dose administered. Its half-life increases in patients with hepatic cirrhosis and end stage renal disease and decrease in case of pulmonary embolism. Hence, its dose should be adjusted in such patients.
- It undergoes degradation mainly by reticuloendothelial system. Inactive metabolites and small amount of undegraded heparin is excreted through urine. It circulates and bound to plasma proteins.
Adverse effects
- Bleeding is the major side effect. Excessive use of heparin may cause bleeding from various sites like kidneys and hemorrhoids, wound hematoma and hemarthrosis. Careful monitoring of patients should be done to prevent bleeding. It may cause thrombocytopenia.
- Long term use of heparin may cause risk of alopecia and osteoporosis. It may cause increase in level of SGOT and SGPT.
- It may cause adverse reactions including fever, chills, urticaria and anaphylactic shock.
Contraindications
Contraindicated in following conditions:
- In patients with known hypersensitivity to heparin or pork products.
- In patients with history of heparin induced thrombocytopenia.
- Patients with risk of bleeding like in people with liver disease, stroke or severe hypertension.
References
- Pharmacology and Pharmacotherapeutics book. 24th edition.
- Goodman and Gillman’s Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology. 6th edition.
- A textbook of Clinical Pharmacology and Therapeutics. 5th edition.
- Page C. Heparin and Related Drugs: Beyond Anticoagulant Activity. ISRN Pharmacol. 2013; 2013: 910743.
- https://www.ncbi.nlm.nih.gov/books/NBK538247/