- Fosfomycin is synthetic derivative of phosphonic acid. It is broad spectrum antibiotic which is produced from organism Streptomyces fradiae. It is also produced synthetically.
- Fosfomycin was discovered in 1969 by researchers of Spanish Penicillin and Antibiotics company.
Antibacterial spectrum of fosfomycin
- It exerts bactericidal action against both gram positive and gram-negative pathogens and is active against Staphylococcus aureus, S. epidermis, Enterococcus faecalis and Enterococcus spp. It is also active against gram-negative pathogens including E. coli, Klebsiella, Citrobacter spp., Shigella spp., Salmonella spp., and Proteus mirabilis.
Indications of fosfomycin
- Used in treating uncomplicated case of cystitis or UTI (urinary Tract Infection) caused by susceptible strains of E. coli and Enterococcus faecalis.
- Its off label uses include in treating pyelonephritis or perinephric abscess.
Mechanism of action of fosfomycin
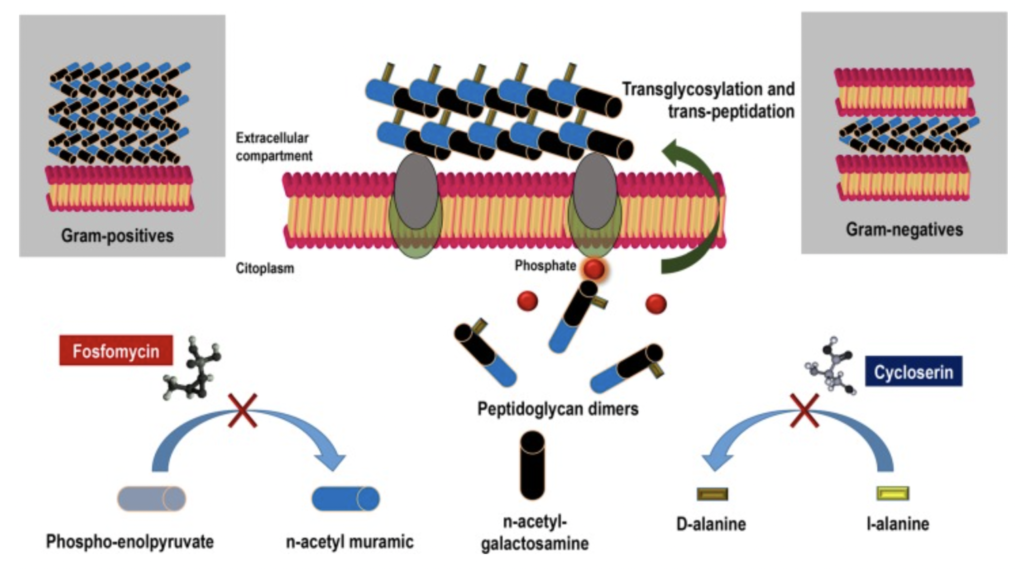
Figure- Mechanism of action of Fosfomycin (Source- Candel et al, 2019)
- It exerts its action by inhibiting bacterial cell wall synthesis.
- The enzyme UDP-N-acetylglucosamine enolpyruvyl transferase (MurA) catalyze transfer of enolpyruvyl moiety of PEP (phosphoenolpyruvate) to 3’ hydroxyl group of UDP-N-acetylglucosamine (U-NAG) leading to formation of peptidoglycan precursor, UDP N-acetylmuramic acid (UDP-MurNAc). Fosfomycin binds to thiol group of a cysteine in active site of MurA and inactivates it resulting in inhibition of UDP-MurNAC formation. Hence, the early step of bacterial cell wall synthesis is disrupted.
- It also affects adhesion of bacteria to urinary epithelial cells.
Pharmacokinetics
- It is well absorbed after oral administration and is also administered by IV route. It is distributed to different tissues including kidney, bladder, lungs, bone, cerebrospinal fluid (CSF) and prostate.
- Very negligible amount of drug binds to plasma proteins. Majority of administered drug is excreted unchanged in urine and little amount is excreted via feces.
- Its half-life is around 4-8 hours. High level in urine persists for more than 48 hours.
- It has low molecular weight compound.
Resistance
- Bacteria may develop resistance to it by different mechanism like:
- Decreased uptake of drug by bacteria due to mutation in genes encoding glycerol-3-phosphate transporter or glucose-6-phopshate transporter which are the major transporter of Fosfomycin.
- Mutation in binding site of target enzyme, MurA.
- Inactivation of fosfomycin by enzymatic cleavage of epoxide ring or by phosphorylation of phosphonate group.
- Some pathogens like Staphylococcus capitis, Staphylococcus saprophylictus, Mycobacterium tuberculosis and Stenotrophomonas maltophilia are intrinsically resistant to it.
Adverse effects
- Some common adverse effects include nausea, headache, diarrhea, and vaginitis. It can also cause rashes, abdominal discomfort, dizziness, drowsiness, and pruritus.
- Prolonged use may result in fungal or bacterial superinfection.
Drug interaction
- It can interact with drugs like lactobacillus acidophilus, bcg vaccine, cholera vaccine, typhoid vaccine, lactobacillus rhamnosus etc.
Contraindications
- Contraindicated in patients with known hypersensitivity to Fosfomycin or other components of the formulation.
- It is pregnancy category B drug.
References
- https://go.drugbank.com/drugs/DB00828
- https://www.drugs.com/drug-interactions/fosfomycin-with-lactobacillus-acidophilus-1139-0-1424-0.html
- Dijkmans AC et al. Fosfomycin: Pharmacological, Clinical and Future Perspectives. Antibiotics (Basel). 2017 Dec; 6(4): 24.
- Falagas ME et al. Fosfomycin. Clin Microbiol Rev. 2016 Apr; 29(2): 321–347.
- Candel FJ et al. New perspectives for reassessing fosfomycin: applicability in current clinical practice. Rev Esp Quimioter. 2019 May; 32(Suppl 1): 1–7.
- A textbook of clinical pharmacology and therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.