- The coronavirus disease 19 (COVID-19) pandemic continues to grow, and as of April 18, 2020, more than 2 million cases have emerged globally. The United States is now the most affected country.
- According to the article published on journal Brain, Behavior and Immunity, researchers have suggested that neuropsychiatric challenges may occur in people recovering from COVID- 19 infections.
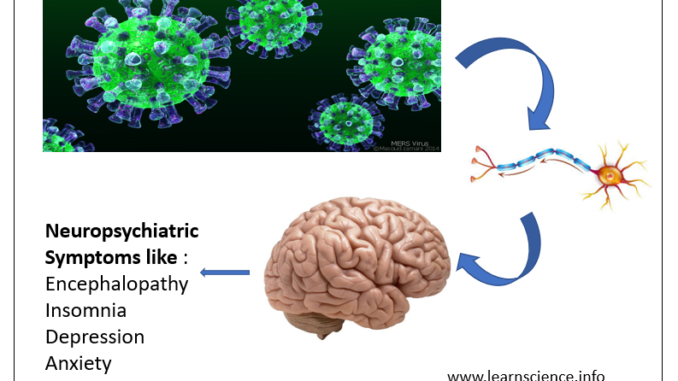
- Past pandemics have shown that various neuropsychiatric symptoms like mood change, psychosis, encephalopathy, neuromuscular dysfunction may occur in recovered patients after weeks, months or longer of viral infection. In 18th and 19th centuries, influenza pandemic occurred which was marked by increased incidence of neuropsychiatric symptoms like insomnia, anxiety, depression, mania and suicidal thoughts. The coronavirus infections (SARS-CoV-1 epidemic) in 2003, influenza pandemic in 2009 and the Middle East respiratory syndrome coronavirus (MERS-CoV) outbreak in 2012 are also marked by several neuropsychiatric sequelae including narcolepsy, seizures, encephalitis, encephalopathy, Guillain-Barre syndrome (GBS), and other neuromuscular and demyelinating processes .
- There are also increasing evidence of acute neuropsychiatric symptoms in COIVD- 19 patients. A study (2019) of 217 hospitalized patients in Wuhan, China, had reported neurologic symptoms including cerebrovascular complications (e.g., stroke), encephalopathies, and muscle injuries in nearly half of those with severe infection (40 of 88).
- According to some reports, SARS-CoV-2 infection is also associated with dysfunction of olfactory and taste perception.
- Exposure to viral infections in utero, during childhood development, and in adulthood have each been associated with increased risk of developing schizophrenia.
- On the other aspect, social isolation, fear of death, illness and uncertainty of future may also affect public mental health.
Potential mechanisms of neuropsychiatric manifestations in COVID-19
- In SARS-CoV-1 patients and experimental animals, the spread of virus from the respiratory tract to the central nervous system (CNS) occur via retrograde axonal transport from peripheral nerves such as the olfactory nerve, or via hematogenous spread. After entering the CNS, CoV has been shown to induce neuronal cell death in mice.
- It has been speculated that the neuroinvasive potential of SARS-CoV-2, particularly of medullary structures involved in respiration (e.g., solitary tract nucleus, nucleus ambiguus), may partially mediate the high incidence of respiratory failure currently seen in COVID-19.
Though, the neuropsychiatric burden of this COVID-19 pandemic is currently unknown, based on past pandemics of this magnitude, the current SARS-CoV-2 pandemic will likely require closer examination of the mechanisms underlying, and the interventions for, post-viral neuropsychiatric sequelae.
Reference
- Emily A.Troyera, Jordan N.Kohna, Suzi Hong. Are we facing a crashing wave of neuropsychiatric sequelae of COVID-19? Neuropsychiatric symptoms and potential immunologic mechanisms. Brain, Behavior and Immunity (2020).
https://www.sciencedirect.com/science/article/pii/S088915912030489X