- Benzodiazepines (BZDs) are a class of medications that work in the central nervous system and are used for treating various medical conditions including anxiety, seizures etc.
- Benzodiazepines have long history of development, starting with the first FDA approval at 1960s. Chlordiazepoxide was the first BZD to get approved. BZDs quickly become popular because of their improved safety profile compared to barbiturates. They have become most widely prescribed pharmacological agents nowadays.
- All BZDs are listed as DEA schedule (Drug Enforcement Administration) IV controlled substance as they have the potential for addiction and abuse.
- Some commonly used BZDs are diazepam, alprazolam, midazolam, nitrazepam, lorazepam, temazepam.
Indications of benzodiazepines
- As hypnotics
- As anticonvulsants
- Used as skeletal muscle relaxant
- In anxiety
- In alcohol withdrawal syndrome
- As pre-anesthetic and anesthetic medication
Mechanism of action of Benzodiazepines
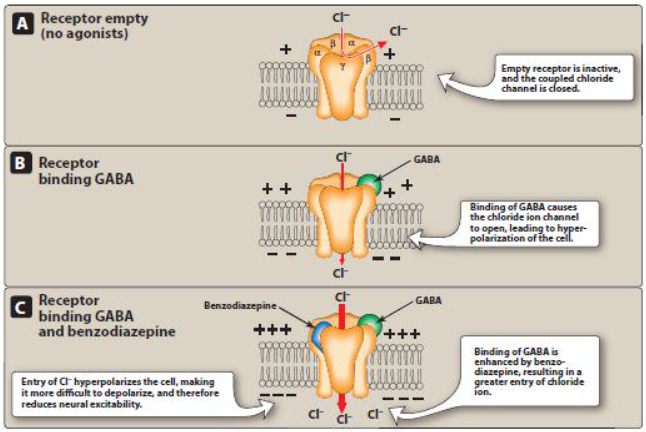
- GABA (Gamma Amino Butyric Acid) is the most common inhibitory neurotransmitter of nervous system. GABAA receptor is a chloride channel formed by 5 subunits comprising varying subtypes to which GABA can binds to and opens chloride channel.
- Benzodiazepine binds to GABAA receptor at sites different from GABA binding site and increases frequency of chloride channel opening resulting in increased neuronal concentration of chloride ion. This causes hyperpolarization of the neuronal membrane and thus make difficult for excitatory neurotransmitters to depolarize the cell.
Pharmacological actions of benzodiazepines
Anxiolytic action
- When chronic, unwarranted worry lasts for a period of six months or longer and interferes with normal daily activities, this may be diagnosed as Generalized Anxiety Disorder (GAD).
- In small doses BDZ reduce aggressiveness and produce relief from anxiety. They have a calming effect.
Sedative-hypnotic action:
- Benzodiazepines when used in large doses, produce sleep.
- Benzodiazepines are preferred as hypnotics because of following reasons:
- They induce more refreshing sleep with less hangover symptoms.
- Can induce sleep even in presence of pain.
- They have high therapeutic index and longer duration of action.
- fewer chances of causing fewer drug interactions.
- They don’t cause significant CVS and respiratory complications even in large doses.
Muscle -relaxant and anti-convulsant action:
- Benzodiazepines like diazepam is useful either alone or in combination to relieve spasticity specially in patients with spinal cord lesion and in cerebral palsy or multiple sclerosis. It reduces painful spasm due to spinal cord lesion.
- Benzodiazepines act as anti-convulsant but are not good choice for long-term treatment of epilepsy.
- Diazepam can be lifesaving in status epilepticus. Status epilepticus is considered a medical emergency in which there is either more than 30 minutes of continuous seizure activity; or there are two or more sequential seizures without recovery of full consciousness between two seizures.
Pre-anesthetic and anesthetic action:
- Short acting benzodiazepines are used either IM or IV for inducing anesthesia. However, it doesn’t produce true general anesthesia, as the awareness and mobility remain.
- It can be used as pre-anesthetic medication along with other anesthetics.
Alcohol Withdrawal Syndrome:
- Benzodiazepines are 1st line treatment for acute alcohol withdrawal. They reduce withdrawal symptoms and may be life saving for patients.
Pharmacokinetics
- Pharmacokinetic characters differ among different benzodiazepines.
- BZDs can be administered through oral, IV, IM, sublingual, rectal or intranasal route. BZDs are metabolized by hepatic microsomal enzymes. Their action may be prolonged in case of hepatic damage.
- Some of BZDs are transformed into clinically active metabolites. BZDs and their metabolites have high protein binding capacity. They are widely distributed in the body and get accumulated in lipid rich areas like adipose tissues and central nervous system. They are excreted through urine.
Adverse Effects
- BZDs are generally well tolerated. Some common side effects are drowsiness, lethargy and ataxia. They can cause daytime sedation, behavioral changes and impairment of visual-motor coordination. Anterograde amnesia (loss of ability to create new memories) may occur with traditional BZDs.
- Long term use may lead to tolerance, dependence and withdrawal effects. Withdrawal syndrome includes insomnia, agitation and convulsion (rarely). The withdrawal symptoms are more intense after withdrawal of short acting BZDs than long acting BZDs.
Drug Interactions
- Serious drug interactions are rare. They may have additive action on CNS depressant activity of alcohol, barbiturates, opioids, MAO inhibitors, antidepressants and phenothiazines if used together. Concomitant use of benzodiazepine with opioids may cause profound sedation, coma and death.
References
- Schmitz Allison. Benzodiazepine use, misuse, and abuse: A review. Mental Health Clinician. 2016; 6(3): 120-126.
- Griffin CE, Kaye AM, Bueno FR, Kaye AD. Benzodiazepine Pharmacology and Central Nervous System–Mediated Effects. Ochsner J. 2013; 13(2): 214–223.
- Pharmacology and Pharmacotherapeutics. 24th edition.