
Alcohol Dependence
- Alcohol abuse is the most common and costly form of drug abuse.
- Continued excessive alcohol consumption lead to the development of alcohol dependence. The development of alcohol dependence is a complex and dynamic process.
- It is a disorder with both genetic and environmental stimulants in which the person continues drinking despite adverse medical or social conditions and ‘desire to drink’ remains uncontrollable and is main interest in their life.
- Neuroadaptive changes due to continued alcohol use and abuse lead to alcohol dependence.
- Harmful alcohol use and alcohol dependence are relatively rare before the age of 15. However, the prevalence increases steeply reaching a peak in the early twenties before declining.
Alcohol Withdrawal
- When an alcohol dependent person abruptly reduces alcohol consumption or stops drinking, withdrawal syndrome may occur. It’s because alcohol suppress CNS activity and like other CNS depressants, withdrawal symptoms are opposite in nature to the effects of intoxication.
- Some clinical features of alcohol withdrawal include rapid heartbeat, shaking, increased blood pressure, excessive sweating and CNS hyperexcitability. Hallucination and delirium may occur in severe form of withdrawal. Emotional changes such as agitation, anxiety, irritation, dysphoria and sleep disturbance may also occur.
Diagnosis of alcohol dependence
- The diagnosis of alcohol dependence is usually made by reviewing the clinical history of patient, but this can be imprecise if the patient is unaware, or reluctant. However, questionnaires can facilitate the process.
- Severity of alcohol dependence can be accessed by using the Severity of Alcohol Dependence Questionnaire (SADQ).
- Below are the diagnostic criteria for alcohol dependence by ICD and DSM.
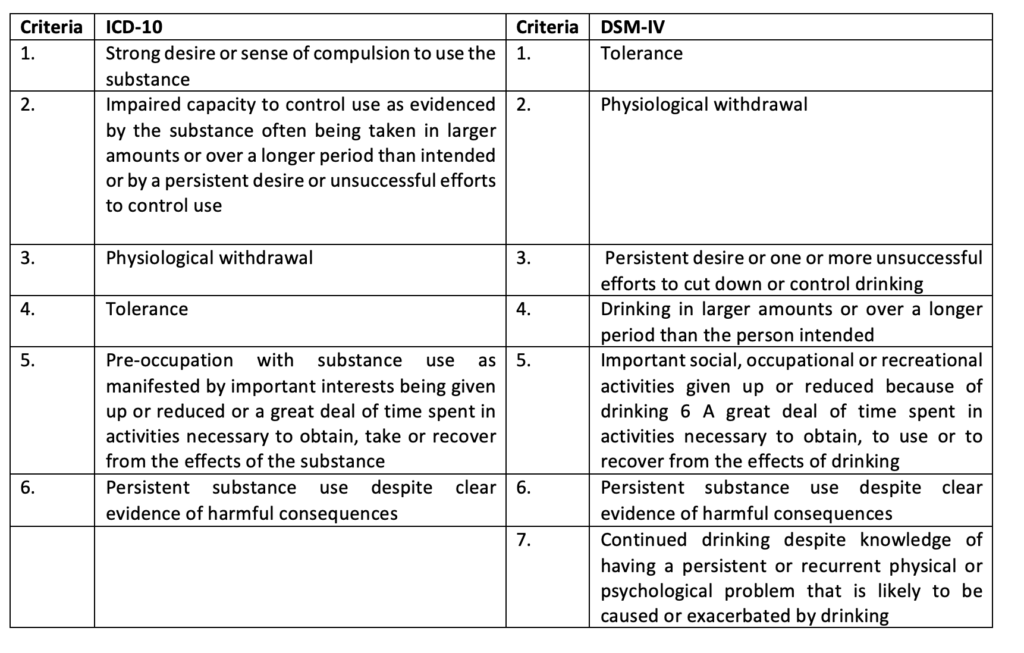
In both the ICD-10 and the DSM-IV criteria, a diagnosis of alcohol dependence is made if three or more of the criteria are present together at some time during the previous 12 months.
Treatment of alcohol dependence
Treatment of alcohol dependence consists of:
- Detoxification
- Support Therapy and
- Rehabilitation
Detoxification
- The initial step in the treatment is withdrawal from alcohol. Detoxification helps in providing safe withdrawal to make the patient alcohol free.
- In some cases, medical assistance may be required to treat withdrawal symptoms.
- Benzodiazepines are most commonly used drugs in this. Long acting benzodiazepines like diazepam or chlordiazepoxide are used. They are given orally every 4-6 hour on the first day, with tapering of doses for the next 5 days.
- Carbamazepine (an antiepileptic drug) can be used as alternative of benzodiazepine. It helps to prevent seizure.
- Chances of nutritional deficiencies like anemia, thiamine deficiency remain. Adequate nutrition and oral multiple B vitamins, including 50–100 mg of thiamine daily is administered. In case of dehydration signs or history of recent bleeding, vomiting, or diarrhea are IV fluids can be given. Glucose is administered IV in case of hypoglycemia.
Support Therapy
- It includes use of anti-craving drugs to support complete abstinence and prevent relapse. The three FDA approved pharmacotherapies for this purpose are disulfiram, naltrexone and acamprosate.
Disulfiram
- It was approved by FDA for treatment of alcohol dependence in 1951.
- Alcohol is metabolized in the liver, via the enzyme alcohol dehydrogenase, to acetaldehyde and then to acetate via the enzyme acetaldehyde dehydrogenase. It inhibits aldehyde dehydrogenase and inhibit oxidation of acetaldehyde. Thus, the level of acetaldehyde increases to toxic level after alcohol ingestion which causes symptoms such as nausea, vomiting, flushing, headache and hypotension. Such unpleasant experiences help to give up drinking.
- Therapy is initiated only if the person has not consumed alcohol for at least 12 hours. The initial dose is 500 mg orally as a single daily dose for 1-2 weeks, followed by 125-250 mg OD (once a day) as the maintenance dose.
- Side effects like headache, drowsiness, lethargy, hepatotoxicity and psychosis may occur.
- It is contraindicated in cardiovascular disease, systemic hypertension, pregnancy/breastfeeding, obvious personality changes in alcoholics. Caution is also advised in the presence of renal failure, hepatic or respiratory disease, diabetes mellitus and epilepsy.
Naltrexone
- Oral naltrexone was FDA approved for alcohol dependence in 1994 and extended release injectable naltrexone in 2006.
- It is an opioid receptor antagonist which blocks opioid receptors and inhibit rewarding effects of alcohol.
- An initial dose of 25 mg/day is recommended increasing over a period of 2 weeks to a maintenance dose of 50 mg/day. Treatment should be continued for 6 months or longer as required. The treatment should be stopped if drinking persists beyond 4–6 weeks. Naltrexone injection can be given once in a month.
- Common side effects associated are nausea, vomiting, dizziness, abdominal pain, reduced appetite, daytime sleepiness. It may cause dose dependent hepatotoxicity.
- Care should be taken to avoid reaction of naltrexone with opioid drugs. Opioids should be stopped 7-10 days before starting treatment. Opioid receptor blockade persists for 48–72 hours after the last oral dose; thus, in an emergency non-opioid analgesic should be used for pain relief. If future use of opioids is anticipated, for example, for elective surgery, then naltrexone should be discontinued ahead of time.
Acamprosate
- It was FDA approved for treating alcohol dependence in 2004.
- Acamprosate is the calcium salt of N-acetyl-homotaurine. Its mechanism is not completely understood till now. It is suggested that it interacts with glutamate neurotransmitter system and reduce severity of withdrawal symptoms including insomnia, anxiety and restlessness. Recently, it had been suggested that it has no direct activity on any neurotransmitter and the therapeutic effects associated to the co-administered calcium moiety.
- Treatment should be started with a daily divided dose of 1998 mg in people weighing >60 kg and of 1332 mg in those weighing <60 kg. Dose adjustment is recommended in people with moderate renal impairment. Treatment should continue for 6 months or longer. It should be stopped if drinking persists beyond 4–6 weeks.
- Adverse effects are usually mild and include headache, diarrhea, rashes.
- It is contraindicated in patients with renal insufficiency as it is excreted through urine.
Rehabilitation
- Treatment therapy for alcohol dependence become more successful if pharmacotherapy is combined with psychotherapy which includes social control, behavioral choice theory, social learning and stress and coping model and institutional therapy.
- Complete cooperation by patient is must in successful treatment so a doctor should explain that indulgence in even small quantities of alcohol again would lead to a relapse. They should be indulged in sports, social or religious activity, education or other goals. Stress and coping therapy aim in building self-confidence and self-efficacy to deal with problematic situations.
- Psychotherapy and drug therapy can be reinforced by institutional therapy (Alcoholics Anonymous, AA) where the patient can interact with the exalcoholics who have become abstainers and are living a happy life. This helps to boost the patient’s morale.
References
- Molina PE, Gardner JD, Smith FMS, Whitaker AM. Alcohol Abuse: Critical Pathophysiological Processes and Contribution to Disease Burden. Physiology (Bethesda). 2014 May; 29(3): 203–215.
- Becker HC. Alcohol Dependence, Withdrawal, and Relapse. Alcohol Res Health. 2008; 31(4): 348–361.
- Hamza DM, Silverstone PH. A Systematic Review of Treatment Modalities for Alcohol Use Disorder. J Subst Abuse Alcohol. 2014; 2(3): 1023.
- Goh ET, Morgan MY. Review article: pharmacotherapy for alcohol dependence – the why, the what and the wherefore. Aliment Pharmacol Ther. 2017; 45: 865–882.
- Pharmacology and Pharmacotherapeutics. 24th edition.