Barbiturate poisoning may occur intentionally to commit suicide or accidentally by use of large dose of drug. The overall hospital mortality rate of barbiturate poisoning is 2 %. If the barbiturate poisoning is severe and patient falls into coma, mortality percentage rises to 15%.
Despite a worldwide decline in barbiturate use, cases of acute poisoning with severe toxicity are still noted, particularly in developing countries. Barbiturates are used as anticonvulsants, for psychiatric uses, to treat certain types of neonatal jaundice and as general anesthetics. The symptoms of acute barbiturate poisoning are:
- depression of CNS, particularly the respiratory system causing decreased breathing and the cardiovascular system causing peripheral circulatory collapse.
- acute renal shutdown
- pulmonary edema
- atelectasis (partial or complete collapse of lungs)
Treatment of acute barbiturate poisoning
Before starting treatment, severity of barbiturate poisoning should be accessed. Presence of reflexes, normal BP and respiration without external assistance indicate better prognosis. Deep coma with cardiovascular collapse, respiratory depression and absence of reflexes indicate high mortality.
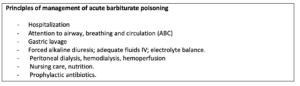
Gastric lavage for Acute Barbiturate Poisoning
In conscious patient if less than 4 hours have elapsed seen ingestion, vomiting can be induced by using concentrated slat solution or ipecac syrup. In unconscious patient, simple aspiration of gastric contents is useful if carried out within 4 hours of barbiturate ingestion. If patient is in coma, endotracheal intubation should precede gastric intubation to prevent aspiration.
Adequate tissue oxygenation:
If the respiration is not affected more, oxygen can be given by nasal catheter. If respiration is affected, endotracheal intubation should be done. In case assisted ventilation is required for more than 24 hours, tracheostomy is usually performed. Frequent monitoring of blood gases and blood pH is helpful. Respiratory physiotherapy helps to minimize lung complications.
Forced diuresis for Acute Barbiturate Poisoning
Diuretics can be used to remove barbiturate from body through increased urinary flow. Commonly used diuretics are mannitol and furosemide. Mannitol is an osmotic diuretic. 25 % solution is given initially in the dose of 100-120 through IV route. Subsequently, a sustained infusion of 5% mannitol alternately in a liter of normal saline and a liter of 5% dextrose is administered at the rate of 500 ml per hour for next 3 hours. After this, depending upon urine output and the state of hydration infusion is adjusted. An average urine volume of 10-12 liters in 24 hours (a flow rate of 8-10 ml per minute) is considered as satisfactory diuresis. The dose of mannitol should not be more than 20 g per hour. Once the patient awakes, diuresis is terminated.Furosemide is a loop diuretic.
Forced diuresis is most useful in poisoning due to phenobarbitone, barbitone and allobarbitone which are more ionized at achievable urine pH. In case of poisoning of barbiturates, which are more protein bound and are less ionized at the achievable urine pH, it many not be effective. Forced diuresis should not be performed if patient is in shock or show cardiac failure and renal impairment. It should only be considered for those patients who have taken phenobarbitone in such doses that they are unlikely to survive with supportive therapy alone. It is not a substitute for the intensive supportive therapy as outlined above as most of the deaths are because of failure to maintain adequate tissue oxygenation.
IV fluids:
IV fluids should be given as an adjuvant to forced diuresis, to maintain blood volume and to prevent dehydration. Normal saline with dextrose can be used.
Dialysis and hemoperfusion:
Hemodialysis, peritoneal dialysis, charcoal hemoperfusion can be used for removing loner acting barbiturates. In patients with severe cardiac and renal impairment, peritoneal dialysis is preferred than forced diuresis. Hemodialysis is about forty times more effective than forced diuresis for barbiturate elimination. Hemodialysis is preferred in following condition:
- In shock
- In patients whom peritoneal dialysis is contraindicated or is not effective.
- Used in case of potentially lethal level of barbiturate in blood
- Progressive deterioration with conservative therapy
Charcoal hemoperfusion is more effective than peritoneal dialysis and hemodialysis.
Alkalinisation of urine:
It is useful in excretion of long acting barbiturates like phenobarbitone. Sodium bicarbonate 3.75g as 50ml of a 7.5% solution may be added to every liter of IV fluid. The urinary pH should be maintained between 7.5 and 8.5.
Prophylactic antibiotics:
They may be required in case if patients need catheterization or tracheostomy.
Prevention of Acute Barbiturate Poisoning
Often, barbiturate poisoning occurs as a result of an irresponsible attitude to the storage of medicines, as well as due to distraction or ignorance. So, it is necessary to store medicines in hard-to-reach places, in a darkened and dry place. One should not rely on own knowledge and skills and prescribe drugs ownself: only a medical specialist can prescribe barbiturate treatment.
If prescribed by a doctor, then during treatment, in no case should alcohol be consumed. Alcohol and barbiturate are incompatible and potentiate each other’s effects. In addition, it is unacceptable to make their own adjustments to the treatment regimen proposed by the doctor.
References
- Norn S, Permin H, Kruse E, Kruse PR. On the history of barbiturates. Dan Medicinhist Arbog. 2015; 43: 133-51.
- Trubuhovich RV. Pioneering early Intensive Care Medicine by the ‘Scandinavian Method’ of treatment for severe acute barbiturate poisoning. Anaesth Intensive Care. 2015 Jul; 43 Suppl: 29-39.
- Darren M. Roberts. Enhanced elimination in acute barbiturate poisoning – A systematic review. Clinical Toxicology. 2011; 49 (1): 2-12.
- Acute poisoning with barbiturates; symptoms, treatments. Accessed on April 9, 2020.
- Pharmacology and pharmacotherapeutics. Page no- 131-134.
- https://www.ncbi.nlm.nih.gov/books/NBK499875/