
- Acetylcholine (Ach) is an organic chemical that function in the body as neurotransmitter. It plays important role in brain and muscle function.
- Acetylcholine is the first neurotransmitter discovered. It was discovered by Henry Hallet Dale in 1914 and later confirmed by Otto Loewi. Both were awarded the Novel prize for their discovery.
- Chemically, it is an ester of choline with acetic acid.
Synthesis of Acetylcholine
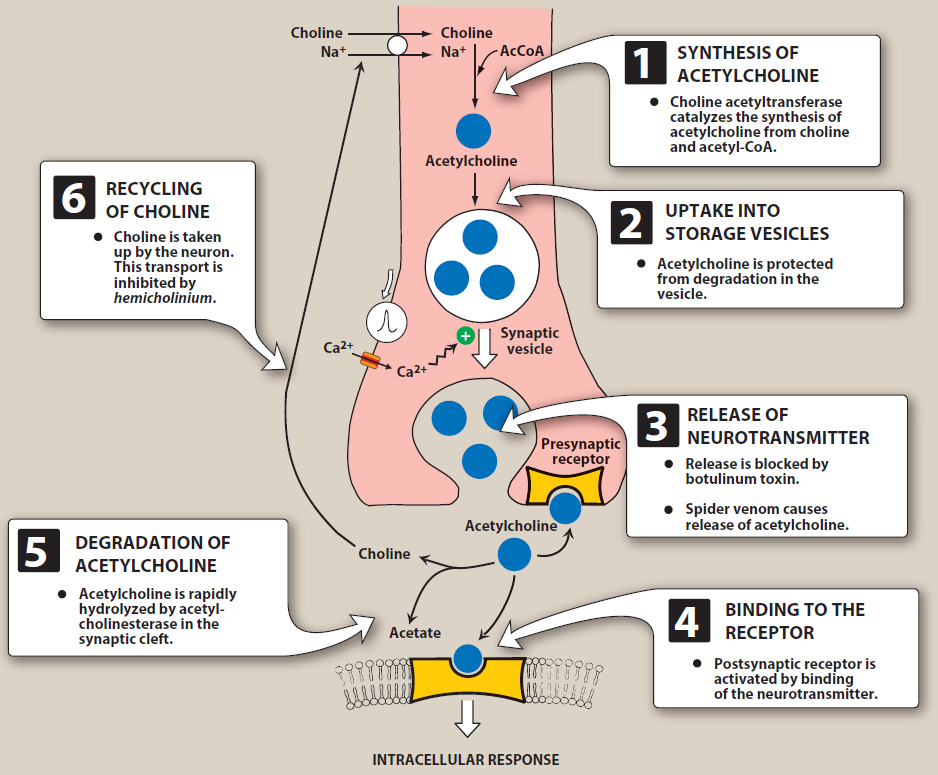
- Choline is transported from extracellular fluid into cholinergic neurons by energy dependent carrier system. In cholinergic neurons, acetylation of choline occurs with acetyl coenzyme A in presence of choline acetyl transferase to form acetylcholine.
- Transport of choline is rate limiting step in Ach synthesis. It depends upon extracellular Na+ and can be inhibited by drug hemicholinium.
Storage and Release of Acetylcholine
- After synthesis, it is stored in storage vesicles at nerve terminals. The vesicles also contain ATP and proteoglycan. Some vesicles may contain peptides that act as co-transmitters.
- A single motor nerve terminal contains 300,000 or more vesicles and Ach content of synaptic vesicle ranges from 1000 to over 50,000 molecules per vesicle.
- It is released by the process of exocytosis. Elevated intracellular calcium level (due to action potential) promote fusion of synaptic vesicle with cell membrane and release of Ach into synaptic gap. This process can be inhibited by botulinum and tetanus toxin.
Acetylcholine Receptors
- The released Ach bind to post synaptic cholinergic receptors. These receptors can be divided into two classes; Muscarinic and Nicotinic receptors.
- Muscarinic receptors are located on tissues supplied by postganglionic parasympathetic nerves, CNS and non-innervated receptor on vascular endothelium. They are of five subtypes- M1, M2, M3, M4 and M5.
- Nicotinic receptors are located on all sympathetic ganglia, adrenals, CNS and skeletal neuromuscular junction.
Pharmacological actions of Ach
Cardiovascular system
- In heart, Ach mimics the action of vagal stimulation. It depresses SA node and causes bradycardia (negative chronotropic action). It decreases contraction (negative ionotropic action).
Blood vessels
- It acts on M3 receptors and dilate blood vessels of mainly skin and mucous membrane. This stimulation cause release of nitric oxide resulting in vascular relaxation. Thus, the blood pressure decreases.
Smooth muscles
- It contracts smooth muscle of gall bladder, urinary bladder, ureter and bronchi (causes bronchospasm). The smooth muscle of uterus shows inconsistent response.
Secretions
- The cholinergic stimulation increases gastric, pancreatic and intestinal secretions. It inceases peristalsis in stomach and the amplitude of digestive contractions. Bronchial, salivary, lacrimal and nasopharyngeal secretions are also augmented.
- The increased bronchial secretion accompanied by bronchospasm may cause cough and dyspnea.
Eye
- Ach causes miosis by contracting circular fibers of sphincter pupillae. It results in reduction of intraocular tension.
- It contracts ciliary muscle which reduces tension on lens, increases its thickness and reduces the focal length. Vision is fixed for a short distance. This is termed as spasm of accommodation.
- Ach (1%) is instilled into anterior chamber of the eye to produce miosis during ophthalmic surgery.
Myoneural junction
- It induces contraction of skeletal muscle. Very high concentration of Ach in myoneural junction can induce paralysis of skeletal muscle.
Miscellaneous actions
- It is a neurohumoral transmitter in the CNS. Cholinergic system is essential for normal behavior and cognition.
- In patients with Alzheimer’s disease and Huntington’s disease significant losses of choline acetyltransferases is detected.
Therapeutic Uses
- When administered orally, it is destroyed in GI tract. When administered through IV route, it is rapidly metabolized by pseudocholinesterase and true cholinesterase.
- Due to its extremely transient action, it cannot be used in clinical practice. So, its substitutes like carbachol, bethanechol and methacholine are used which are effective orally, more selective and directly acts as Ach receptor agonist.
Degradation of Ach
- Ach is cleaved by acetylcholinesterase to choline and acetate in synaptic cleft. Choline may be recaptured by sodium-coupled, high affinity uptake system that transports the molecule back into the neuron.
References
- Pharmacology and Pharmacotherapeutics. 24th edition.
- Goodman and Gillman Manual of Pharmacology and Therapeutics.
- Lippincott Illustrated Reviews Pharmacology, 6th edition.
- Brown DA. Acetylcholine. Br J Pharmacol. 2006 Jan; 147(Suppl 1): S120–S126.
- Neuron. Author manuscript; available in PMC 2013 Oct 4.
- Picciotto MR, Higley MJ, Mineur YS. Acetylcholine as a neuromodulator: cholinergic signaling shapes nervous system function and behavior. Neuron. 2012; 76(1): 116–129.
- https://www.medicalnewstoday.com/articles/326638