Local anesthetics
- Local anesthesia is loss of sensation in a body part without the loss of consciousness or the impairment of central control of vital functions. Local anesthetics are drugs which when applied directly to peripheral nerves, blocks nerve conduction and abolish all sensation in the part supplied by that nerve. It can cause both sensory and motor paralysis in the area innervated.
- They are different from general anesthetics.
Mechanism of action of local anesthetics
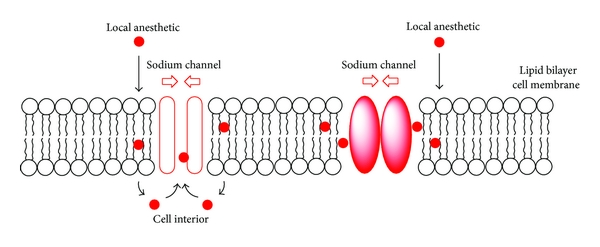
- Sodium ion channels which initiate the action potential in electrically excitable cells are the molecular targets of local anesthetic drugs. Local anesthetics bind reversibly to receptors present near the intracellular end of voltage gated Na+ channels. This prevent the increase in permeability of cell membrane to Na+ ion (first event of depolarization) which leads to blockade of action potential generation. Thus, it blocks both generation and conduction of nerve impulse. Local anesthetics can block K+ channels at higher concentration of drug, blockade of conduction is not accompanied by change in resting membrane potential.
- This action affecting the process of depolarization, leading to failure of impulse propagation without affecting the resting potential, is known as membrane stabilizing effect.
Figure- Mechanism of local anesthetics
Classification of Local anesthetics
- Natural: Cocaine
- Synthetic Nitrogenous Compound:
I) Para-amino benzoic acid derivatives- e.g. Procaine, Benzocain
II) Acetanilide derivatives- e.g. Lignocaine
III) Acridine derivatives- e.g. Bucricain
IV) Quinoline derivatives- e.g. Cinchocaine
- Synthetic non-nitrogenous Compounds: e.g., Benzyl alcohol, Propanediol
- Miscellaneous: e.g., Antihistamines like diphenhydramine, Clove oil, Phenol
General Properties of Local Anesthetics
- Synthetic local anesthetic drugs have many common properties. Structurally, local anesthetics have specific fundamental features in common. These include
- A lipophilic aromatic group joined by an
- An intermediate chain (amide or ester linkage to a carbon chain) which in turn is joined to
- A hydrophilic amino group
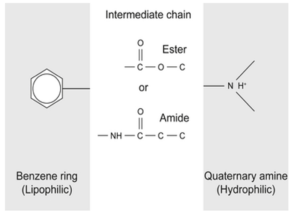
Figure: General structure of local anesthetics
- Due to the presence of amino nitrogen, they act as bases and form water soluble salt with acids. In the tissues, where the pH is alkaline, free base is liberated and produce its pharmacological actions.
- They possess varying degree of water and lipid solubility. Lipid solubility helps the drug to move into neuronal fiber and water solubility helps in movement of drug from site of injection to site of action. Thus, the local anesthetics with high lipid but low water solubility will not be much useful because of difficulty in transportation through aqueous phase.

Figure: Structure of some local anesthetics
Onset and duration
- Factors affecting onset and duration of action
- pH of tissue
- pKa of the drug
- Nerve morphology
- Time of diffusion from needle tip to nerve and time of diffusion away from nerve
- Concentration of drug
- Lipid and water solubility of drug
- The most important factors affecting onset are pH of the tissue and pKa of the drug. The pH may drop in site of infection, which causes onset to be delayed or even prevented.
- The duration of action depends on the length of time the drug stays in nerve to block the sodium channels. Local anesthetics cause vasodilation, which leads to rapid diffusion away from site of action resulting in very short duration of action when administered alone. This diffusion can be reduced by adding vasoconstrictor, usually epinephrine.
Method of administration of local anesthetics
Topical anesthesia:
- Anesthesia of mucous membrane of body parts like mouth, nose, throat, genitourinary tract can be produced by direct application of aqueous solution or suspension of local anesthetic. e.g. Amethocaine is used as surface anesthetic for the eye, throat, rectum, skin and urethra. Dibucaine is used for rectum, skin and ear. Tetracaine and proparacaine are used exclusively for eye.
- Following topical application to denuded skin or mucous membrane, they are rapidly absorbed into circulation which may produce systemic toxic reactions.
Infiltration anesthesia:
- In this procedure, nerve endings are anesthetized by their direct exposure to drugs. It can be so superficial as to include only the skin or it can also include deeper structures, including intra-abdominal organs. e.g. Procaine 2% and lignocaine 2% are commonly used. They are mixed with adrenaline to prolong their action. The advantage of infiltration anesthesia is it can produce sufficient anesthesia without disrupting normal body function. Its chief disadvantage is relatively large amount of drugs must be used to anesthetize relatively small areas.
Spinal anesthesia:
- In this procedure, the drug is injected into sub-arachnoid space. Lignocaine and bupivacaine are the most commonly used drugs. It is one of the most popular form of anesthesia. The position of the patient is important in limiting the block to desired level. One of the most important side effects of anesthesia is hypotension which can be treated by using vasopressor drugs, rapid intravenous infusion of fluids and elevation of the legs.
Epidural anesthesia:
- It is administered by injecting local anesthetic into the epidural space. Its current popularity arises from the development of catheters that can be placed into epidural space, allowing either continuous infusion or repeated bolus administration of local anesthetic. In this case, spread of anesthetic is restricted to a specific region and hence have fewer complications. Lidocaine are bupivacaine are commonly used. The duration of action can be increased, and side effects can be decreased by adding epinephrine.
Nerve block or conduction block anesthesia:
- Local anesthetic is not intentionally injected directly into nerves as it is painful and may cause nerve damage. So, the drug is injected very close to nerve e.g. brachial plexus. The areas of sensory and motor block usually start several centimeters distal to the site of injection. Choice of the anesthetic is determined by the duration of anesthesia needed.
Adverse effects of local anesthetics
- Central Nervous System: They may cause CNS stimulation producing restlessness and tremor that may lead to clonic convulsion. CNS stimulation is followed by depression. Lignocaine may produce dysphoria or euphoria, loss of consciousness. This effect can be countered by using preanesthetic diazepam.
- Cardiovascular System: Electrical excitability, force of contraction and conduction rate may decrease. Lower doses of local anesthetics may cause cardiovascular collapse and death, rarely. Hypotension may occur.
- Allergic reactions: Ester local anesthetics are more allergic than amides. This may manifest as allergic dermatitis, asthmatic attack and severe anaphylactoid reaction.
- Methemoglobinemia: It is mostly associated with prilocaine and with articaine or benzocaine. So, they are avoided in patients with congenital methemoglobinemia. It is induced by an excess metabolite of these drugs.
- Systemic toxicity: High blood level of drug may be due to repeated administration or single inadvertent intravascular administration. The signs and symptoms of toxicity are vomiting, hyperventilation, syncope etc.
References
- Daniel A. Huss. An Update on Local Anesthetics in Dentistry. J Can Dent Assoc. 68(9):546-51.
- DS Ragsdale, JC McPhee, T Scheuer, WA Catterall. Molecular determinants of state-dependent block of Na+ channels by local anesthetics. Science. 265(5179):1724-1728.
- Reynolds. Adverse Effects of Local Anesthetics. Br. J. Anaesth. 59:78-95.
- Pharmacology and Pharmacotherapeutics book, R.S. Satoskar. Page no- 257-262.
- Goodman and GILLMAN’S Manual of Pharmacology and Therapeutics. Page no- 241-252.
- A textbook of Clinical Pharmacology and Therapeutics. Page no -152-154.
- https://en.wikipedia.org/wiki/Local_anesthetic